Blood Thinners: What They Are, How They Work, and What You Need to Know
When your blood clots too easily, it can lead to strokes, heart attacks, or pulmonary embolisms. That’s where blood thinners, medications that reduce the blood’s ability to form clots. Also known as anticoagulants, they don’t actually thin your blood—they slow down the clotting process so clots don’t grow or break loose. If you’ve been prescribed one, you’re not alone. Millions take them after heart surgery, for atrial fibrillation, or after a deep vein thrombosis. But knowing how they work isn’t enough—you need to know what can mess them up.
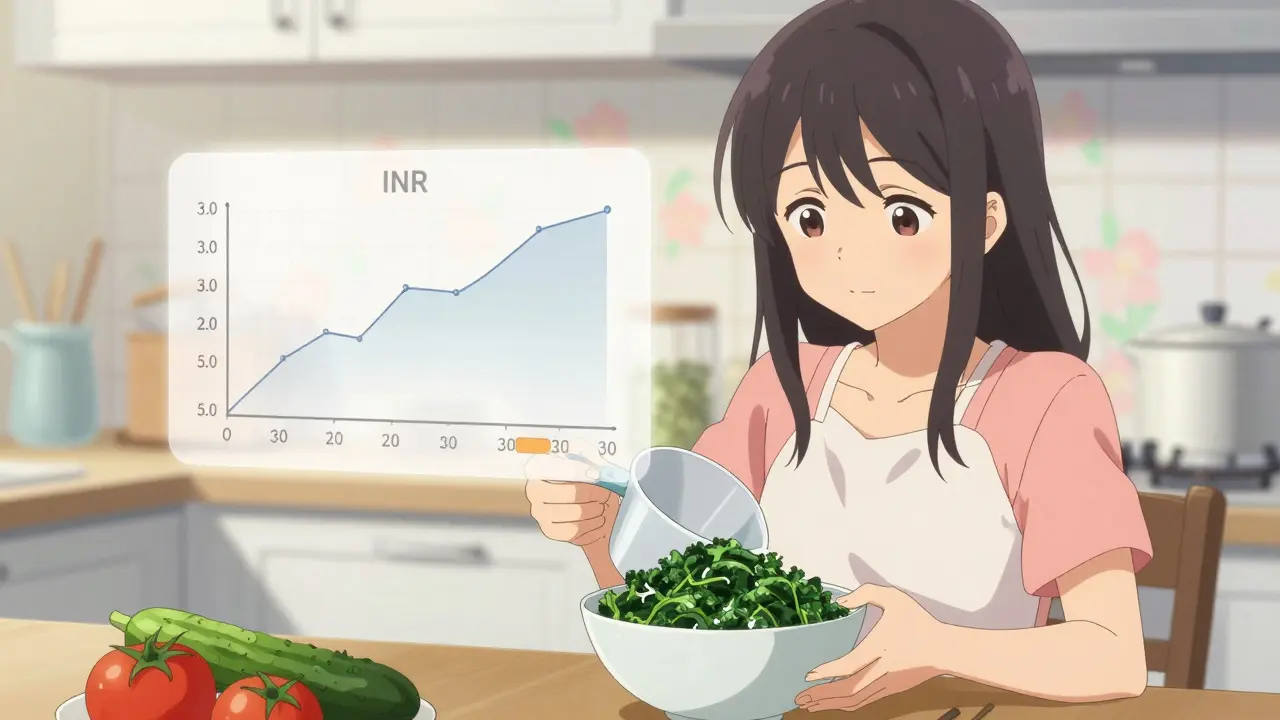
Not all blood thinners are the same. warfarin, an older anticoagulant that requires regular blood tests works by blocking vitamin K, which your body needs to make clotting factors. That’s why foods like kale and broccoli can throw your dose off. Then there are newer ones like apixaban or rivaroxaban—they don’t need routine blood checks, but they still interact with other drugs. And if you’re on INR monitoring, a test that measures how long it takes your blood to clot, even small changes in diet, supplements, or other meds can push your number too high or too low. A high INR means you’re at risk of bleeding. A low one means clots could form. There’s no middle ground.
Some of the most dangerous interactions happen with common drugs. Phenytoin, an epilepsy med, can make warfarin less effective. Antibiotics like ciprofloxacin can spike your INR. Even over-the-counter painkillers like ibuprofen can increase bleeding risk. And don’t forget herbal stuff—ashwagandha, ginkgo, garlic supplements—they all play a role. That’s why keeping a clear, updated list of everything you take isn’t just smart, it’s lifesaving. Medical alert bracelets? They’re not just for show. In an emergency, if you can’t speak, that bracelet tells responders you’re on a blood thinner—and that changes everything.
You’ll find posts here that dig into real-world problems: how warfarin interacts with phenytoin, why your INR keeps swinging, what to avoid when you’re on anticoagulants, and how to spot pharmacy errors with generics. You’ll learn how to read your lab results, what to do if you miss a dose, and why some people need to wear ID bracelets while others don’t. These aren’t theoretical discussions—they’re based on what actually happens in clinics, pharmacies, and ERs. Whether you’re taking a blood thinner yourself, caring for someone who does, or just trying to understand the risks, this collection gives you the facts you need to stay safe.
Green Leafy Vegetables and Warfarin: Why Consistency Beats Avoidance
Warfarin patients don't need to avoid green leafy vegetables-just eat the same amount every week. Learn how vitamin K affects blood thinning, which greens are safe, and why consistency beats avoidance for stable INR levels.

Perioperative Management of Anticoagulants: How to Safely Handle Blood Thinners Before and After Surgery
Learn how to safely manage blood thinners before and after surgery with updated guidelines for DOACs and warfarin. Avoid bleeding and clot risks with clear timing rules, reversal options, and practical checklists.

Dental Procedures on Blood Thinners: What You Need to Know About Bleeding Risk and Safety
Learn the latest guidelines on dental procedures while on blood thinners. Discover when to stop or keep your anticoagulants, how to prevent bleeding, and what your dentist should do to keep you safe.

Ginkgo Biloba and Blood Thinners: What You Need to Know About Bleeding Risk
Ginkgo biloba can increase bleeding risk when taken with blood thinners like warfarin, aspirin, or clopidogrel. Learn the real dangers, who should avoid it, and what to do if you're already combining them.

Blood Thinners and NSAIDs: Why This Combination Can Cause Life-Threatening Bleeding
Combining blood thinners with NSAIDs like ibuprofen or naproxen can double or even quadruple your risk of dangerous internal bleeding. Learn why this common drug mix is so risky-and what safer alternatives actually work.
