Dental Procedure Safety Calculator
Procedure Safety Assessment
Safety Assessment Results
Procedure Risk Level
Key recommendations
Important warning: This procedure may require special precautions. Consult your dentist and prescribing physician immediately.
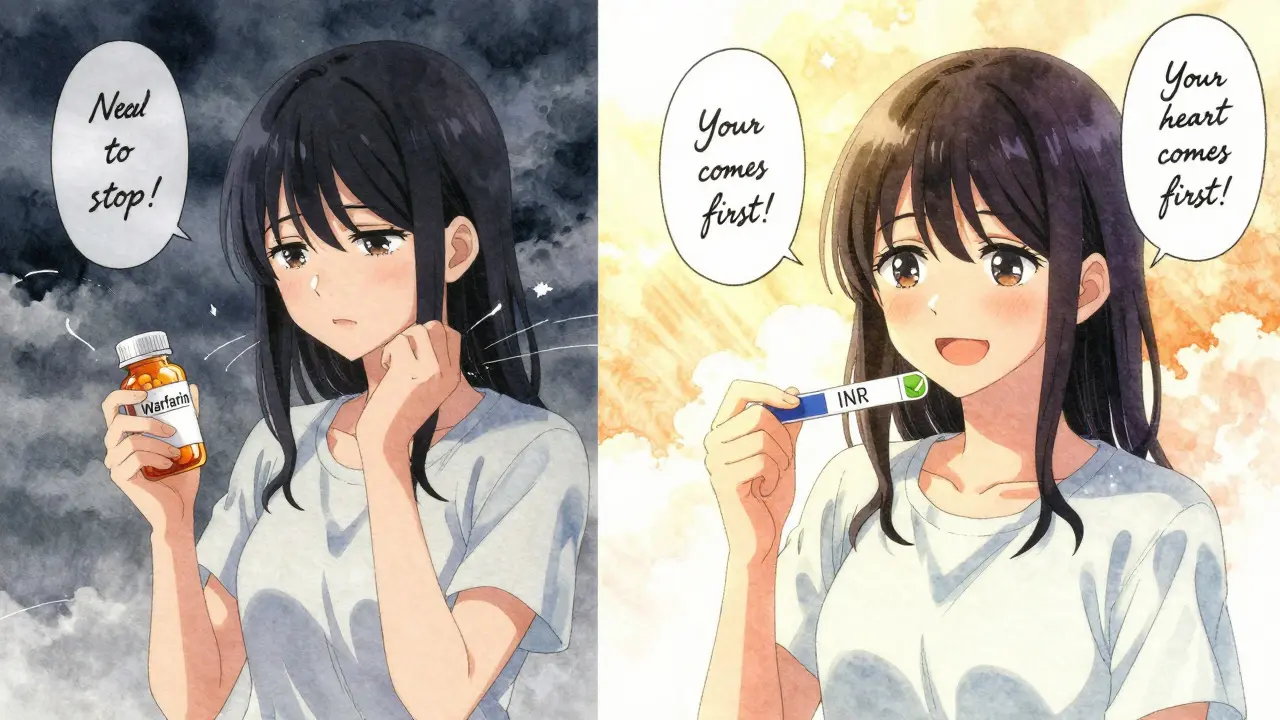
Getting a tooth pulled or a deep cleaning while on blood thinners can feel scary. You’ve probably heard stories about people bleeding for hours after dental work. But here’s the truth: most dental procedures are perfectly safe even if you’re on anticoagulants. The real danger isn’t the bleeding-it’s stopping your medication unnecessarily.
Why Stopping Blood Thinners Is Often More Dangerous
For years, dentists would tell patients to stop their blood thinners before any procedure. That’s no longer the standard. In fact, stopping these medications can be life-threatening. Studies show that pausing warfarin or DOACs (direct oral anticoagulants) for even a few days increases the risk of stroke, heart attack, or blood clots in the lungs. The risk of a clot forming is far greater than the risk of extra bleeding from a simple filling or extraction.The American Dental Association (ADA) updated its guidelines in 2022 to make this clear: For most dental procedures, you should keep taking your blood thinner exactly as prescribed. This isn’t just a suggestion-it’s backed by data from thousands of patients. A 2023 study from UCSD Health found that minor dental procedures cause almost no major bleeding when anticoagulants are continued. The same study showed that stopping them didn’t reduce bleeding, but did raise clot risk by up to 8%.
How Dental Procedures Are Classified by Bleeding Risk
Not all dental work is the same. Bleeding risk is broken down into three levels:- Low-risk procedures: Routine cleanings, X-rays, fillings, crowns, root canals. These cause minimal bleeding. No need to adjust your meds.
- Low-moderate risk: Scaling and root planing (deep cleaning), single tooth extractions. Still very safe with blood thinners. Most patients don’t need to pause their medication.
- Moderate risk: Removing 2-3 teeth, gum surgery, bone removal, complex extractions. These require more planning, but even here, stopping your blood thinner is rarely needed.
Stanford Health Care and the Scottish Dental Clinical Effectiveness Programme (SDCEP) both agree: if the procedure is low or low-moderate risk, keep taking your blood thinner. Only moderate-risk cases might need a short hold-and even then, only after checking with your doctor.
Warfarin vs. DOACs: Different Rules, Same Goal
There are two main types of blood thinners: warfarin (an older VKA) and DOACs like apixaban, rivaroxaban, or dabigatran. DOACs now make up about 60% of new prescriptions because they’re easier to manage and don’t need regular blood tests.For warfarin users: Your doctor checks your INR level (a blood test that measures clotting time). If your INR is under 3.5, you’re fine for most procedures. For single extractions, keep your INR under 3. If it’s above 3.5, your dentist should consult your prescribing physician before proceeding.
For DOAC users: No blood tests are needed. The guideline is simple: skip your morning dose on the day of the procedure if it’s a moderate-risk surgery. For simple cleanings or fillings, take your dose as usual. Wait at least 4 hours after your last dose before the procedure to let the drug clear from your system. This reduces bleeding without raising clot risk.
What Your Dentist Should Do to Prevent Bleeding
Even if you’re on blood thinners, your dentist has tools to control bleeding. Here’s what they should use:- Tranexamic acid mouthwash: A 5% solution you swish for 1-2 minutes, then spit. Repeat every 2 hours if needed. This isn’t magic-it’s a clot-stabilizing agent proven to reduce bleeding by over 50% in anticoagulated patients.
- Pressure and sutures: A gauze pack held firmly for 30-60 minutes after extraction is often enough. Stitches may be used to close the socket.
- Avoid multiple extractions: Don’t pull three teeth in one sitting. Space them out over two or three visits. This gives your body time to heal and reduces overall bleeding.
- No NSAIDs: Avoid ibuprofen, naproxen, or aspirin after the procedure. These can increase bleeding. Use acetaminophen (Tylenol) for pain instead.
Also, avoid smoking, drinking through a straw, or rinsing vigorously for 24 hours. These actions can dislodge the clot and cause a dry socket-even more dangerous if you’re on anticoagulants.
Red Flags: When to Call Your Dentist or Doctor
Most bleeding stops within a few hours. But if you notice any of these, act fast:- Bleeding that doesn’t stop after 2-3 hours of pressure
- Swallowing large amounts of blood (more than a few teaspoons)
- Feeling dizzy, weak, or short of breath
- Swelling that gets worse after 24 hours
If you’re on warfarin and your INR is above 4.0, or if you’re taking DOACs and have kidney or liver disease, your risk is higher. Always tell your dentist about all your medications-including over-the-counter supplements like fish oil, ginkgo, or garlic pills. These can thin your blood too.

Special Cases: Younger Patients and Pregnancy
You might think blood thinners are only for older people with heart conditions. Not anymore. More young adults are on them now: a 28-year-old recovering from a pulmonary embolism after childbirth, a 32-year-old athlete with atrial fibrillation, or a 25-year-old with a genetic clotting disorder. These patients need the same careful planning-but sometimes with extra caution.Pregnant women on anticoagulants require special attention. Warfarin can harm the fetus, so many switch to heparin during pregnancy. Dental work is still safe, but your OB and dentist must coordinate. DOACs are generally avoided in pregnancy, so your treatment plan will be tailored.
What You Should Do Before Your Appointment
Don’t wait until the day of your cleaning to think about this. Here’s your checklist:- Make a list of every medication you take-including dose and frequency.
- Know your INR if you’re on warfarin. Bring your last lab result.
- Ask your prescribing doctor if you should stop your blood thinner. Most will say no.
- Inform your dentist you’re on anticoagulants. Don’t assume they know.
- Ask if they use tranexamic acid mouthwash. If they don’t, ask why.
Many dentists now follow ADA guidelines, but not all. A 2022 survey found 78% of U.S. dental practices use current anticoagulation protocols. That’s good-but you still need to advocate for yourself.
Bottom Line: You Don’t Have to Choose Between Your Teeth and Your Heart
The old advice-stop your blood thinner before dental work-is outdated and dangerous. Modern guidelines say: keep taking your meds. Most dental procedures are low-risk and can be done safely without interruption. The key is communication: between you, your dentist, and your prescribing doctor.Bleeding from a tooth extraction isn’t usually a crisis. But a stroke caused by skipping your medication? That’s life-changing. You’re not taking a risk by keeping your blood thinner. You’re protecting yourself.
Can I get a tooth pulled while on blood thinners?
Yes, most single tooth extractions are safe while on blood thinners. Your dentist will use local measures like pressure, sutures, or tranexamic acid mouthwash to control bleeding. You usually don’t need to stop your medication. Only in rare cases-like multiple extractions or complex surgery-might your doctor recommend a short pause, and even then, only after evaluating your clotting risk.
Should I stop warfarin before a dental cleaning?
No. Routine cleanings are low-risk procedures. Stopping warfarin increases your chance of stroke or clot without reducing bleeding. As long as your INR is under 3.5, you can safely proceed. Always bring your latest INR result to your appointment.
Do DOACs require different dental precautions than warfarin?
Yes. DOACs like apixaban or rivaroxaban don’t need blood tests, but timing matters. For moderate procedures, skip your morning dose and wait at least 4 hours after your last dose before the procedure. For cleanings or fillings, take your dose as usual. DOACs leave your system faster than warfarin, so short holds are safer and more effective.
What painkillers are safe after dental work if I’m on blood thinners?
Use acetaminophen (Tylenol). Avoid NSAIDs like ibuprofen, naproxen, or aspirin-they interfere with platelet function and increase bleeding risk. Even low-dose aspirin can be risky if you’re already on anticoagulants. Always check with your doctor before taking anything new.
How long should I wait to resume my blood thinner after a tooth extraction?
If you skipped a dose before the procedure, restart your medication as soon as bleeding is controlled-usually within 24 hours. For warfarin, restart the same day unless your doctor says otherwise. For DOACs, resume your next scheduled dose. Delaying too long increases clot risk. Never wait more than 24 hours without consulting your prescriber.
Can I use mouthwash after a dental procedure if I’m on blood thinners?
Yes-but avoid alcohol-based mouthwashes. They can irritate the extraction site and delay healing. Instead, use a saline rinse or a prescribed tranexamic acid solution. These help control bleeding without disrupting the clot. Avoid vigorous rinsing for at least 24 hours.


Jacob Cathro
January 20, 2026 AT 05:57bro i got a root canal last month on warfarin and my mouth was GUSHING like a broken fire hydrant. dentist just shrugged and said ‘eh, it’s fine’ - then handed me a whole box of gauze. i swear i swallowed half a cup of blood. why do they even let this happen? 🤡
Paul Barnes
January 21, 2026 AT 21:28The ADA’s 2022 guidelines are unequivocal: anticoagulant continuation is standard of care for low- and low-moderate-risk dental procedures. Discontinuation increases thrombotic events without reducing hemorrhagic complications, as demonstrated in multiple meta-analyses including the 2023 UCSD Health cohort study. Patient safety hinges on adherence to evidence-based protocols, not anecdotal fear.
pragya mishra
January 21, 2026 AT 23:43Why are you all just accepting this? My cousin died after a tooth extraction because they didn’t stop his blood thinner. You think a guideline is more important than a life? Dentists are just trying to save time - they don’t care if you bleed out. Someone needs to sue someone.
Manoj Kumar Billigunta
January 22, 2026 AT 04:12This is actually really helpful. I’m on rivaroxaban and was terrified to get my wisdom teeth out. I didn’t know skipping the morning dose was enough. I told my dentist about this and they were surprised I knew - they actually used tranexamic acid mouthwash, which I didn’t even know existed. Thanks for the clarity. Just remember: your doctor and dentist need to talk. Don’t assume they already did.
sagar sanadi
January 23, 2026 AT 01:59They say don’t stop your meds… but what if the whole thing’s a pharma scam? Warfarin and DOACs make billions. What if bleeding isn’t the problem - what if they just want you to keep buying pills so you never heal? Ever think about that? They told us aspirin was good for you too. Remember that?
kumar kc
January 24, 2026 AT 10:39Stop being lazy. If you’re on blood thinners, you should’ve read this before you even booked the appointment. This isn’t hard. You’re not special. Just follow the damn guidelines.
Carolyn Rose Meszaros
January 24, 2026 AT 11:12OMG I just got my first deep cleaning last week and I was SO nervous 😭 I asked if they used tranexamic acid and they were like ‘oh yeah, we always do!’ I cried a little. Also I got a free mint! 🌿🦷
Greg Robertson
January 25, 2026 AT 09:34Just wanted to say thanks for writing this. My mom’s on warfarin and I’ve been trying to get her to stop skipping her dentist appointments. She thought she had to choose between her heart and her teeth. This post made it way easier to explain why she doesn’t. I printed it out for her.
Nadia Watson
January 26, 2026 AT 00:29It is imperative to underscore the critical importance of interprofessional communication between dental practitioners and prescribing physicians, particularly in the context of anticoagulant therapy management. While the evidence base supporting continued anticoagulation is robust, the implementation gap persists due to fragmented care models and inconsistent patient education. A standardized, documented handoff protocol - ideally with electronic health record integration - would significantly mitigate risk and enhance outcomes.
Courtney Carra
January 26, 2026 AT 07:38It’s funny how we fear the body’s natural response - bleeding - but ignore the silent, invisible crisis of clotting. We’re taught to fear the visible wound, not the invisible storm. Maybe the real question isn’t ‘Can I get my tooth pulled?’ but ‘Can we trust modern medicine to not turn healing into a gamble?’