Drug Absorption: How Your Body Takes in Medication and Why It Matters
When you swallow a pill, it doesn’t just disappear and start working. Drug absorption, the process by which a medication enters your bloodstream from the site of administration. Also known as medication uptake, it’s the first step that decides whether your drug will do its job—or sit there useless. If absorption is poor, even the most powerful medicine won’t help. That’s why two people taking the same pill can have totally different results—one feels relief fast, the other feels nothing.
Drug absorption isn’t just about swallowing. It’s shaped by bioavailability, the percentage of a drug that actually reaches circulation. A drug with 90% bioavailability works better than one with 30%, even if they’re the same dose. Factors like stomach acid, food in your gut, or even the pill’s coating can slash absorption. For example, calcium supplements can block thyroid meds like levothyroxine if taken together. Same with iron and antibiotics—timing matters more than you think.
Then there’s drug interactions, when one substance changes how another is absorbed. Phenytoin can speed up how fast your body breaks down warfarin, making your blood thinner than intended. Ashwagandha might boost thyroid hormone levels, pushing someone on thyroid medication into dangerous over-replacement. These aren’t rare edge cases—they happen daily, often because patients don’t know how food, supplements, or other pills interfere.
Some drugs are designed to absorb slowly—extended-release versions of blood pressure meds, for instance. Others need an empty stomach. If you take your antibiotic with dairy, you might as well throw it away. The same goes for certain painkillers or antidepressants. Even the pH of your gut can change absorption. That’s why your pharmacist asks if you eat breakfast before taking your meds.
And it’s not just about pills. Patches, injections, inhalers—all have their own absorption rules. A skin patch delivers medicine steadily, but sweat or heat can mess with it. An inhaler needs perfect technique or the drug hits your throat instead of your lungs. If you’ve ever wondered why your medication feels less effective after a few weeks, poor absorption might be why.
This collection of articles dives into exactly how these processes play out in real life. You’ll find guides on how to time your meds to avoid interference, how to spot when your generic pill isn’t working like it should, and why some drugs need to be taken with food while others absolutely can’t. We cover what happens when supplements like ashwagandha or calcium clash with prescriptions, how packaging and labeling affect whether you’re getting real medicine, and how pharmacy errors can sabotage absorption without anyone noticing.
Whether you’re managing a chronic condition, caring for an elderly parent, or just trying to make your meds work better, understanding drug absorption gives you real control. It’s not magic—it’s science. And once you know how it works, you can ask the right questions, spot red flags, and finally get the results you’re paying for.

Fexofenadine and Fruit Juice: Why Your Allergy Medicine Might Not Be Working
Fexofenadine (Allegra) loses up to 77% of its effectiveness when taken with grapefruit, orange, or apple juice due to blocked absorption. Here's why, and what to do instead.
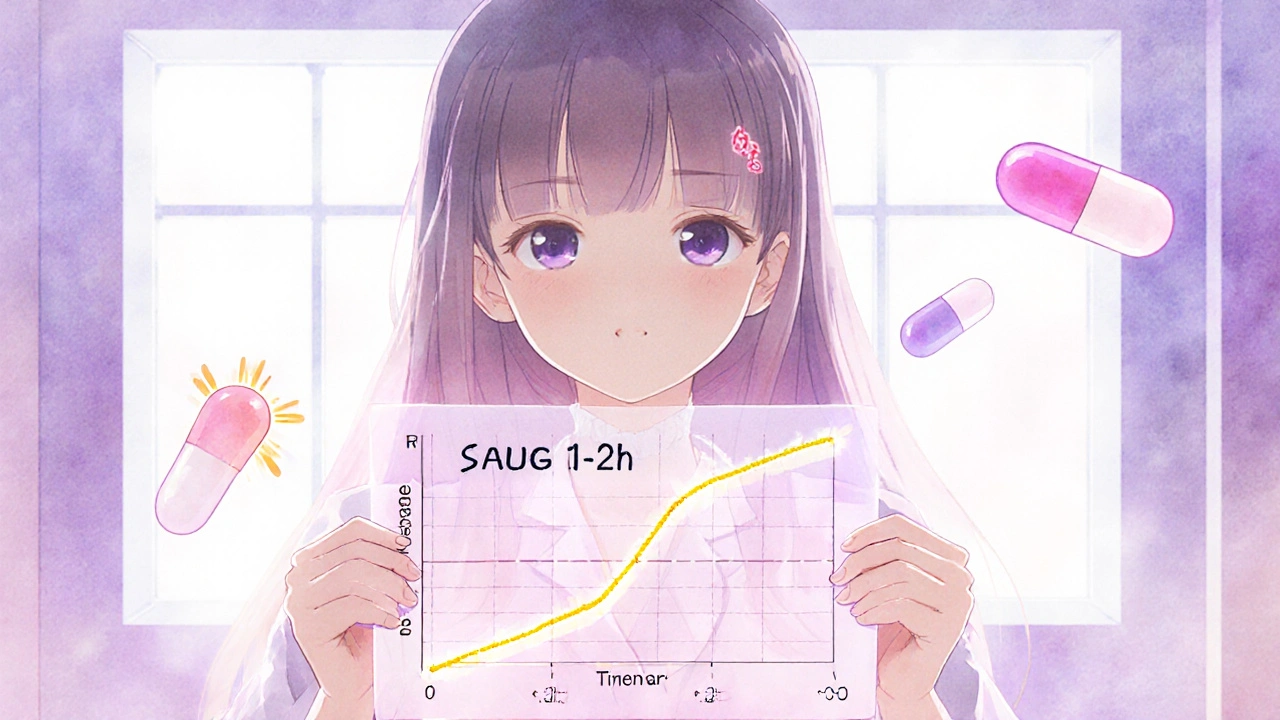
Partial AUC in Bioequivalence: How Advanced Metrics Ensure Drug Safety and Effectiveness
Partial AUC is a precise pharmacokinetic tool used to ensure generic drugs match brand-name versions in how quickly they're absorbed. It's now required for complex formulations like extended-release opioids and CNS drugs.
