Bioequivalence: What It Means for Generic Drugs and Your Health
When you pick up a generic pill, you’re counting on it to do the same job as the brand-name version—that’s where bioequivalence, the scientific standard proving two drugs deliver the same amount of active ingredient at the same rate in the body. Also known as therapeutic equivalence, it’s the reason your pharmacist can legally swap your prescription without asking your doctor. This isn’t guesswork. The FDA requires bioequivalence testing before any generic drug hits the shelf. That means if your brand-name drug releases 90% of its active ingredient into your bloodstream within two hours, the generic must do the same—within a tight, scientifically proven range.
But bioequivalence isn’t just about the active ingredient. It’s also about how fast and how completely your body absorbs it. Two pills might have identical ingredients, but if one dissolves slowly and the other quickly, they won’t behave the same in your system. That’s why bioequivalence studies measure blood levels over time, not just total amount. This matters most for drugs with narrow therapeutic windows—like warfarin, thyroid meds, or epilepsy treatments—where even small differences can cause side effects or make the drug stop working. You’ll find posts here that dig into real cases where bioequivalence got tested, from pharmacy errors with generics to how formulary changes affect what you get at the counter.
Not all generic switches are equal. Some manufacturers cut corners on inactive ingredients, which can change how a pill breaks down. That’s why packaging, labeling, and even the shape of the tablet can hint at quality. The FDA doesn’t approve every generic the same way—some get fast-tracked, others face inspections. And overseas manufacturing issues? They’ve led to warning letters and recalls. You’ll see posts here that show you how to spot red flags in your meds, what to do if your insurance drops your drug, and why therapeutic interchange (switching within the same drug class) still relies on bioequivalence as its foundation.
What you’ll find below isn’t theory. It’s real-world stories: how a patient’s INR swung after switching phenytoin generics, why ashwagandha can mess with thyroid meds even if they’re bioequivalent, and how calcium supplements can block absorption even when the drug itself is perfectly matched. These aren’t edge cases—they’re common pitfalls that happen because bioequivalence doesn’t guarantee identical behavior in every body. You’re not just buying a cheaper pill. You’re trusting a system that’s supposed to keep you safe. Below, you’ll find guides that help you understand that system, question it when needed, and protect yourself when things go off-track.
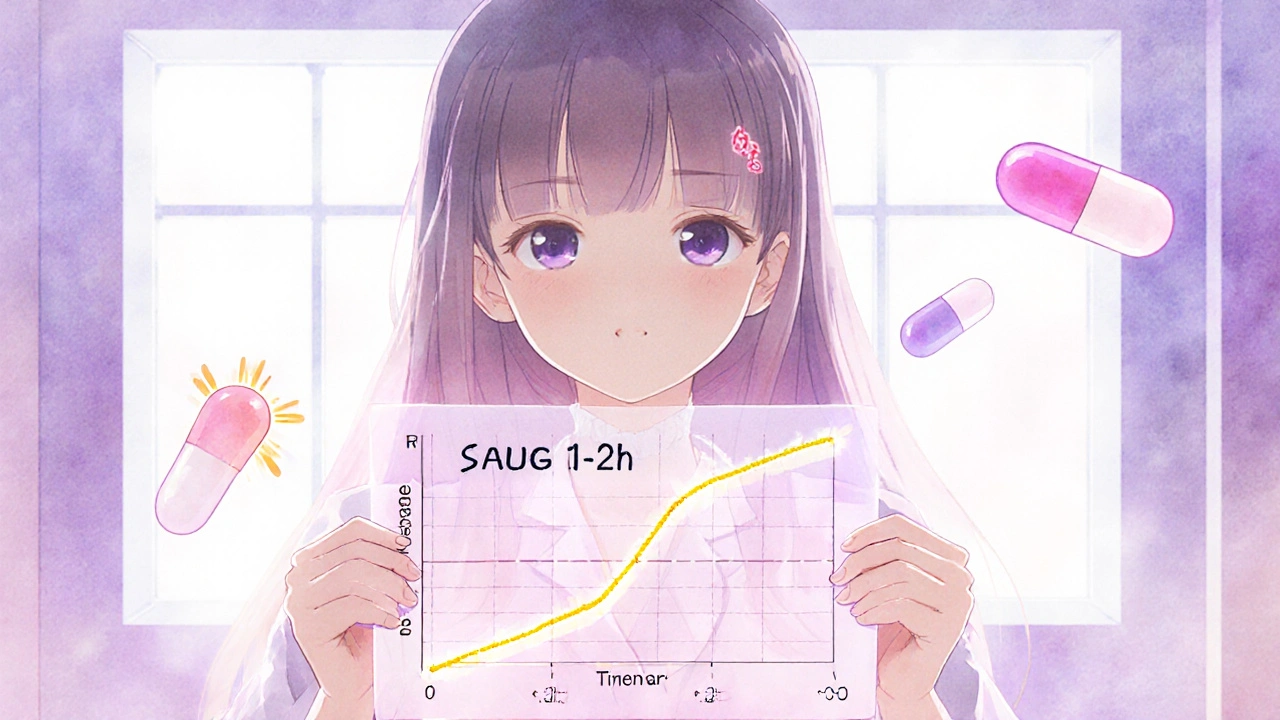
Partial AUC in Bioequivalence: How Advanced Metrics Ensure Drug Safety and Effectiveness
Partial AUC is a precise pharmacokinetic tool used to ensure generic drugs match brand-name versions in how quickly they're absorbed. It's now required for complex formulations like extended-release opioids and CNS drugs.
