Why Renal Ultrasound Is the First Step When Kidneys Are Suspected to Be Blocked
When a patient shows up with severe flank pain, nausea, or reduced urine output, doctors don’t jump straight to a CT scan. They start with a renal ultrasound. Why? Because it’s fast, safe, and tells you almost everything you need to know about kidney blockage and size-without radiation, contrast dye, or long waits.
Imagine a patient with a kidney stone stuck in the ureter. The urine backs up, causing the kidney to swell-a condition called hydronephrosis. On a CT scan, you see the stone. On an ultrasound, you see the swelling. And sometimes, that’s all you need to know. In emergency rooms across the U.S., point-of-care ultrasound cuts diagnosis time by nearly 45 minutes compared to waiting for a formal CT. That’s not just convenience; it’s better care.
What Exactly Does a Renal Ultrasound Show?
Renal ultrasound doesn’t just take pictures. It measures. And those numbers matter.
Doctors look at three key things:
- Kidney size: Normal adult kidneys are 9 to 13 centimeters long. If one is significantly smaller, it could mean chronic damage. If both are enlarged, it might point to something like polycystic kidney disease.
- Cortical thickness: The outer layer of the kidney (the cortex) should be at least 1 cm thick. Thinning means scarring from long-term pressure or disease.
- Hydronephrosis: This is the swelling caused by backed-up urine. It’s graded from mild to severe using the Society for Fetal Urology system. Mild means just a little dilation in the center of the kidney. Severe means the whole kidney looks like a water balloon.
They also check the renal pelvis-the funnel-shaped part where urine collects before flowing into the ureter. A normal anteroposterior diameter is less than 7 mm. Anything above that raises a red flag.
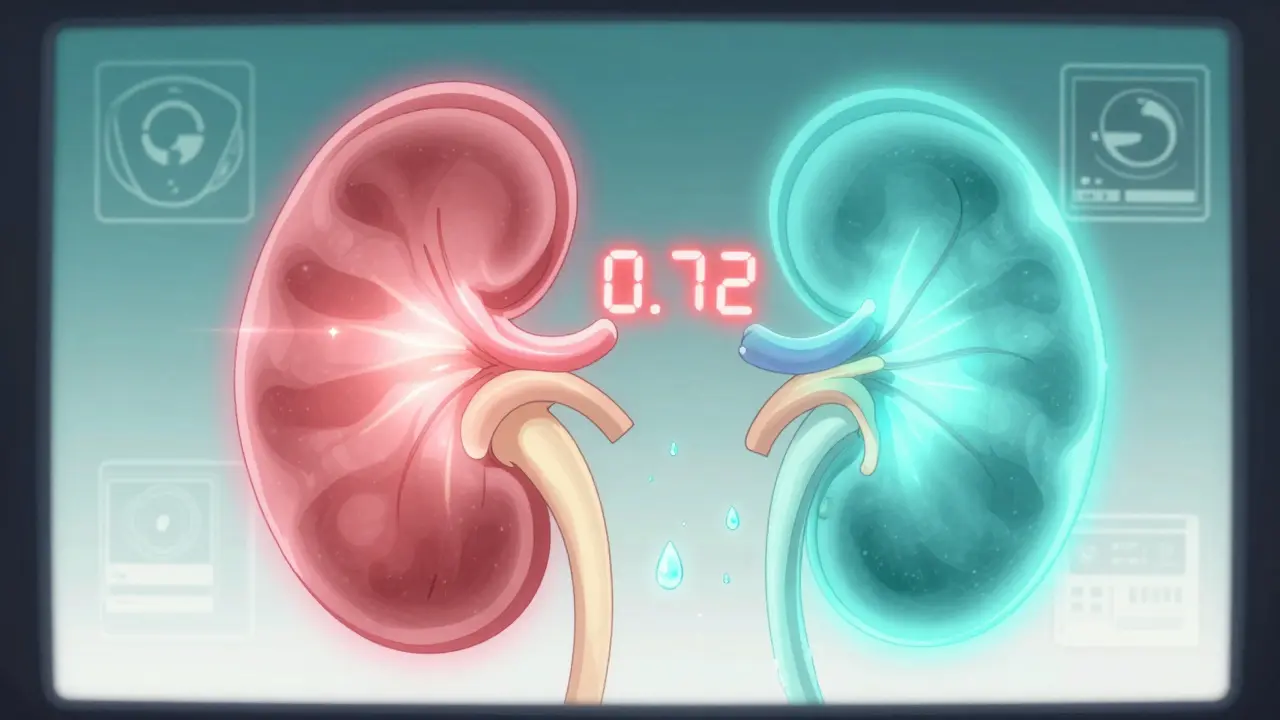
The Resistive Index: A Hidden Clue to Blockage
Here’s where ultrasound gets smart. It doesn’t just show structure-it shows blood flow.
Using Doppler ultrasound, technicians measure the resistive index (RI) in the interlobar arteries inside the kidney. The formula is simple: (Peak Systolic Velocity - End Diastolic Velocity) ÷ Peak Systolic Velocity.
What does that number mean? An RI below 0.70 is normal. Above 0.70? That’s a strong indicator of obstruction. A 2015 study in the Nigerian Journal of Clinical Practice found that an RI of 0.70 or higher had 86.7% sensitivity and 90% specificity for detecting obstructive uropathy. That’s better than many blood tests.
Why does this work? When urine backs up, pressure builds inside the kidney. That pressure squeezes the tiny blood vessels, making it harder for blood to flow out during diastole. The result? A higher RI. It’s not perfect-but it’s one of the most reliable non-invasive signs of obstruction.
Ultrasound vs. CT vs. MRI: What’s the Real Difference?
People often ask: “If CT scans show stones so clearly, why use ultrasound at all?”
Here’s the truth: CT scans are great for finding small stones-down to 1 or 2 mm. But they expose you to about 10 millisieverts of radiation. That’s like 3 years of natural background radiation. And if you need repeated scans-say, to track a stone’s progress-you’re stacking up exposure.
Ultrasound doesn’t see tiny stones as well. It picks up about 80% of stones larger than 3 mm. But it sees the effect of the stone: the swelling, the backup, the pressure. And that’s often enough to guide treatment.
MRU (Magnetic Resonance Urography) gives detailed pictures of the urinary tract and no radiation-but it costs 3 to 5 times more than ultrasound, takes longer, and still misses small stones. Nuclear scans show kidney function but involve radiation and give blurry anatomy.
Bottom line: Ultrasound is the first step because it answers the most urgent questions safely. If it’s inconclusive, then you move to CT or MRI. Not the other way around.
When Ultrasound Fails-And What Comes Next
Ultrasound isn’t magic. It has limits.
Obesity is the biggest problem. When a patient’s BMI is over 35, sound waves can’t penetrate deep enough. The image gets blurry, measurements become unreliable. In those cases, doctors switch to CT or MRI-even if it means more radiation or higher cost.
Another issue? Operator skill. A 2018 study found that novice sonographers could vary kidney length measurements by up to 20% compared to experts. That’s why training matters. The American Institute of Ultrasound in Medicine (AIUM) recommends at least 40 supervised exams before someone is considered competent. And even then, interpretation takes experience.
Also, bowel gas can block the view. Patients aren’t asked to fast, but if their intestines are full of air, the kidneys might be hidden. In those cases, repositioning the patient or waiting a few hours helps.
What’s New in Kidney Ultrasound? Elastography and AI
Ultrasound isn’t standing still. New techniques are making it even more powerful.
Shear-wave elastography measures how stiff the kidney tissue is. When urine is blocked, pressure builds-and the kidney gets stiffer. Studies show a direct link between increasing pressure and rising stiffness. This could one day let doctors measure obstruction severity without invasive tests.
Then there’s super-resolution ultrasound and ultrasound localization microscopy. These experimental techniques are starting to visualize tiny blood vessels in the kidney. Imagine being able to see early signs of kidney damage-before function declines. That’s the future.
Hospitals like Mayo Clinic are already testing AI-powered hydronephrosis grading. Instead of a radiologist eyeballing dilation, software analyzes the image and gives a consistent, automated score. Early results show it matches expert readings closely.
These aren’t science fiction. They’re rolling out now. And they’ll make ultrasound even more essential.
Who Gets a Renal Ultrasound-and When?
It’s not just for people with kidney stones. Here’s who benefits:
- Patients with sudden flank pain, especially if they’re pregnant (CT is avoided due to fetal radiation risk)
- Children with suspected urinary tract obstruction-ultrasound is the gold standard here
- People with recurrent urinary infections and unknown cause
- Post-surgical patients (e.g., after UPJ repair) needing weekly monitoring
- Those with high blood pressure and reduced kidney function, to check for structural causes
And in emergency departments? If someone comes in with suspected renal colic, ultrasound is the first test. The American College of Radiology rates it as “usually appropriate” for this scenario-higher than CT.
What to Expect During the Exam
The test takes 15 to 30 minutes. No fasting. No needles. No radiation.
You’ll lie on your back or side. A gel is applied to your flank or abdomen. The technician moves a handheld probe over your skin. You might be asked to hold your breath or change position to get better views.
Doppler will be used to check blood flow. You’ll hear a whooshing sound-that’s the blood moving through your kidney arteries.
Results are often available the same day. In emergency settings, the doctor may get the findings within minutes.
How Accurate Is It? Real Numbers
Let’s get specific:
- Sensitivity for detecting hydronephrosis: 95% or higher
- Specificity for obstruction: 88-92% when using RI ≥ 0.70
- Accuracy for detecting stones >3 mm: ~80%
- Reduction in radiation exposure compared to CT: Up to 95%
- Cost per exam (U.S.): $200-$500 (CT urography: $1,000-$2,500)
It’s not perfect-but it’s the best balance of safety, speed, and usefulness we have.
Why This Matters for Long-Term Kidney Health
Untreated obstruction doesn’t just cause pain. It causes permanent damage. If urine backs up for weeks or months, the kidney tissue starts to die. That’s irreversible.
Ultrasound catches this early. It lets doctors intervene-remove a stone, place a stent, or schedule surgery-before the kidney is permanently injured.
And because it’s safe, it’s ideal for follow-up. A patient with a known UPJ obstruction can be monitored every few weeks with ultrasound. No radiation buildup. No contrast risks. Just clear, repeated measurements showing if things are improving or worsening.
Can renal ultrasound detect kidney stones?
Yes, but not all of them. Ultrasound detects about 80% of kidney stones larger than 3 mm. Smaller stones (1-2 mm) are often missed. That’s why CT is still used if the diagnosis is unclear or if a small stone is suspected. But ultrasound doesn’t just look for stones-it shows the swelling caused by them, which is often more important for treatment decisions.
Is renal ultrasound safe during pregnancy?
Absolutely. Unlike CT or X-rays, ultrasound uses sound waves, not radiation. It’s the preferred imaging method for pregnant women with suspected kidney stones or obstruction. It’s safe for both mother and baby and can be repeated as needed without risk.
What does a high resistive index mean?
A resistive index (RI) of 0.70 or higher suggests increased resistance to blood flow in the kidney, often due to obstruction. It’s not a standalone diagnosis, but when combined with hydronephrosis and clinical symptoms, it strongly points to urinary blockage. Values above 0.75 are highly suggestive of significant obstruction.
Can obesity affect the accuracy of a renal ultrasound?
Yes. When a patient has a BMI over 35, sound waves struggle to reach the kidneys through thick abdominal tissue. Images become blurry, measurements unreliable. In these cases, doctors often turn to CT or MRI, even though they involve radiation or higher cost. Weight isn’t a barrier to the test, but it can limit its usefulness.
Do I need to prepare for a renal ultrasound?
No special preparation is needed. You don’t have to fast. But being well-hydrated helps. A full bladder can improve the view of the lower ureters and bladder, so your provider might ask you to drink water before the exam. Otherwise, just show up as you are.
How often can someone have a renal ultrasound?
As often as needed. Because it uses no radiation or contrast, there’s no limit. Patients with chronic obstruction, post-surgical recovery, or kidney transplants often get ultrasounds weekly or monthly to track changes. It’s the safest tool for long-term monitoring.
Is renal ultrasound used for children?
Yes-it’s the primary imaging tool for children with suspected urinary tract obstruction. It’s especially useful for diagnosing conditions like ureteropelvic junction (UPJ) obstruction. Higher-frequency probes are used for smaller bodies, and the test is quick, painless, and avoids radiation exposure entirely.
What’s the difference between hydronephrosis and hydroureter?
Hydronephrosis is swelling of the kidney due to urine backup. Hydroureter is swelling of the ureter-the tube that carries urine from the kidney to the bladder. They often occur together, but ultrasound can distinguish them. Seeing hydronephrosis without hydroureter suggests a blockage near the kidney. Seeing both suggests a blockage lower down, maybe near the bladder.
Final Thoughts: Why Ultrasound Won’t Be Replaced
CT scans are faster for finding stones. MRIs give prettier pictures. But neither is as safe, as cheap, or as repeatable as ultrasound.
Renal ultrasound is the quiet workhorse of kidney imaging. It doesn’t need fancy machines or contrast agents. It works in ambulances, ERs, and rural clinics. It’s used in newborns and elderly patients alike.
With AI and elastography pushing its limits, it’s not just surviving-it’s evolving. In 2026, if your doctor orders a renal ultrasound, it’s not because they’re cutting corners. It’s because they know it’s the smartest first step.


Harriot Rockey
February 4, 2026 AT 07:14Love how this breaks down ultrasound into something actually useful instead of just another tech buzzword. I’m a nurse in the ER and we’ve seen patients wait 3 hours for a CT only to find out the stone was tiny and they just needed fluids and ibuprofen. Ultrasound saves time, money, and sanity. 🙌
Roshan Gudhe
February 5, 2026 AT 14:07There’s a quiet poetry in how medicine returns to simplicity-sound waves revealing the hidden, no radiation, no cost, no hype. Ultrasound doesn’t shout; it listens. And in a world obsessed with spectacle, that’s revolutionary.
Janice Williams
February 5, 2026 AT 19:53Let’s be honest-this is just another attempt to glorify outdated technology because hospitals are too cheap to buy proper imaging equipment. CT scans are objectively superior in every measurable way. The fact that you’re defending ultrasound like it’s some sacred ritual is embarrassing.
rahulkumar maurya
February 6, 2026 AT 06:15One must question the epistemological foundation of relying on operator-dependent modalities in an age of algorithmic precision. Ultrasound, while charmingly analog, lacks the ontological certainty of CT’s voxel-based topology. The RI metric? A heuristic masquerading as a biomarker. One wonders if this is medicine-or folklore with a transducer.
Samuel Bradway
February 6, 2026 AT 10:27I had a kidney stone last year and they did the ultrasound first. Honestly? It was way less scary than I thought. No needles, no noise, just some gel and a weird little wand. The tech even showed me the swelling on the screen. Felt like magic.
Caleb Sutton
February 7, 2026 AT 18:10They’re hiding the truth. Ultrasound is being pushed because Big Pharma and the FDA don’t want you knowing CT scans cause cancer. They’re sacrificing your kidneys for profit. Read the studies-radiation isn’t ‘safe’ just because it’s ‘low dose.’
Jamillah Rodriguez
February 9, 2026 AT 16:20Okay but why does everyone act like this is news? I’ve had 3 ultrasounds in 5 years. It’s just… a thing. Also, the guy who wrote this clearly loves his Doppler. 😴
Susheel Sharma
February 10, 2026 AT 04:27While the piece is commendable in its pedagogical intent, it suffers from a profound lack of critical engagement with the limitations of shear-wave elastography’s inter-observer variability. The AI grading claims? Pre-validated on curated datasets-real-world performance remains unproven. This reads like a vendor whitepaper dressed as clinical guidance.
Rachel Kipps
February 11, 2026 AT 04:48really helpful info… i had no idea about the resistive index thing. kinda blew my mind. also, i think the part about obesity affecting the image is super important, esp for people like me who’ve been told ‘we can’t see well enough’ before. thanks for writing this.
Coy Huffman
February 12, 2026 AT 06:05bro this is why i love medicine sometimes. no fancy machines, just a smart doc with a probe and a brain. ultrasound is the OG diagnostic tool. ai? cool. elastography? hype. but the hand on the belly? that’s real.
Kunal Kaushik
February 13, 2026 AT 18:01My dad had a stone last year. Ultrasound caught it, no radiation, no stress. He’s 72 and still hikes every weekend. This stuff matters. 🙏
Mandy Vodak-Marotta
February 14, 2026 AT 03:44Okay but can we talk about how wild it is that we’re using something invented in the 1950s to make decisions that used to require million-dollar machines? Like, imagine if your phone’s camera was still the one from 2008 and suddenly it could take 8K photos with AI zoom and no internet. That’s ultrasound. It’s not broken-it’s just been quietly upgrading under the hood. Also, the part about bowel gas hiding the kidneys? YES. My cousin’s ultrasound got canceled because she ate beans the night before. She was so mad. Beans are the real enemy of modern medicine.
Nathan King
February 15, 2026 AT 11:35The assertion that ultrasound is ‘the first step’ is not universally valid. In tertiary care centers with immediate CT access, the diagnostic yield and speed of non-contrast CT for acute flank pain exceeds that of ultrasound, particularly in obese populations or when differential diagnosis includes appendicitis, diverticulitis, or aortic pathology. The recommendation to defer CT risks misdiagnosis. This is not evidence-based-it is dogma.
Alec Stewart Stewart
February 16, 2026 AT 03:14Just wanted to say thank you for writing this. My sister’s a med student and she’s been stressing about learning all this. I showed her your post-she said it finally made sense. You made something complicated feel human. 🤍