Every year, thousands of patients in Australia and around the world get the wrong dose, the wrong brand, or even the wrong drug - not because of a doctor’s mistake, but because of a simple mix-up with a generic medication. Generics make up over 90% of prescriptions filled in pharmacies. They’re cheaper, widely used, and just as effective as brand-name drugs - in theory. But in practice, they come with hidden risks that most patients don’t know about, and many pharmacists struggle to catch.
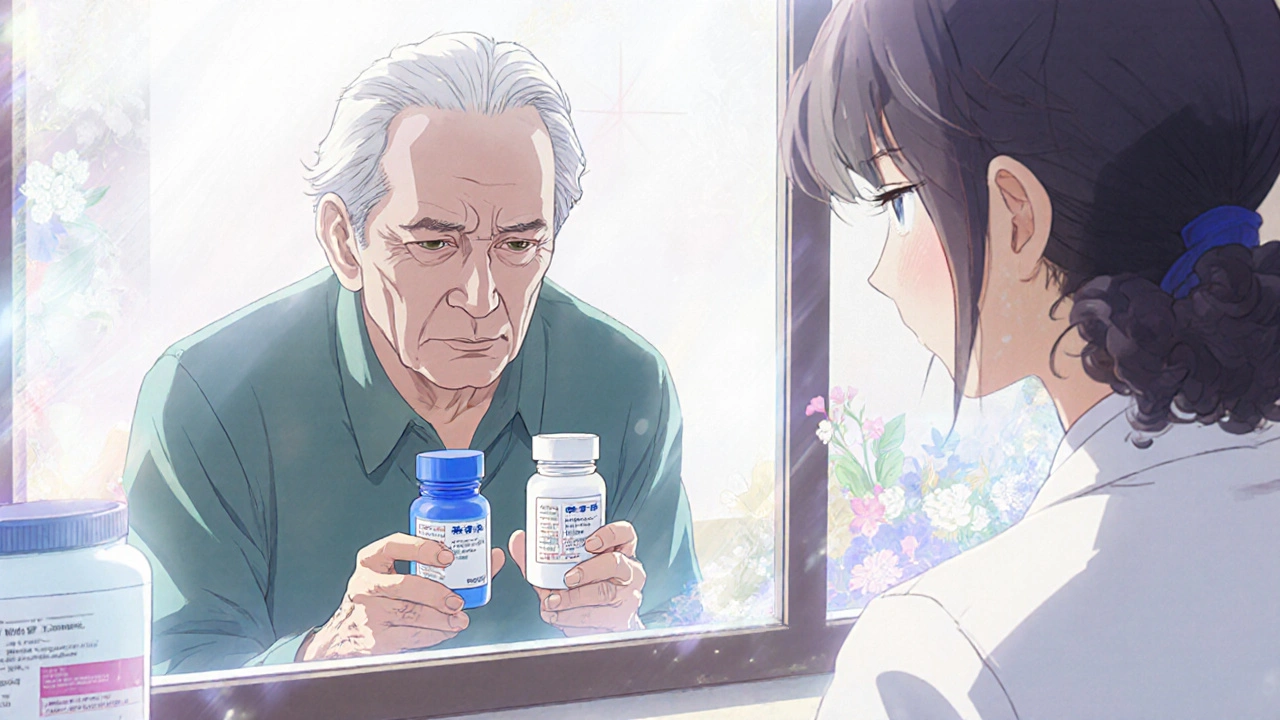
Imagine this: a 68-year-old man takes his daily blood pressure pill. He’s been on the same generic lisinopril for two years. One day, his pharmacist swaps the bottle. The new pills are smaller, white instead of blue, and have a different imprint. He doesn’t say anything. He takes them. Two days later, he feels dizzy, his blood pressure spikes, and he ends up in the ER. The new generic? Bioequivalent. But it had a different filler - and his body reacted. This isn’t rare. It happens more often than you think.
Why Generics Are More Likely to Cause Errors
Generics aren’t just cheaper copies. They’re made by dozens of different manufacturers, each with their own look, size, color, and inactive ingredients. The FDA requires them to be 80-125% as absorbed as the brand name. That’s a huge range. Two generics of the same drug can behave differently in your body - especially if you’re elderly, have kidney issues, or take multiple meds.
Here’s the real problem: pharmacists don’t always know which version is which. Drug databases are outdated. A 2023 survey found that 42% of community pharmacies in the U.S. still use reference guides with old manufacturer details. In Australia, where generic substitution is common, pharmacists often don’t get notified when a new batch comes in - unless the patient complains.
Look-alike, sound-alike names make it worse. Amlodipine vs. Amiodarone. Metoprolol vs. Methylphenidate. One typo, one misread script, and you’ve given someone a heart drug instead of a blood pressure pill. These errors aren’t always caught by computer systems. Many pharmacy software programs don’t flag generic substitutions unless they’re set up specifically for it - and most aren’t.
The Most Common Generic Medication Errors
Based on real pharmacy data from over 400,000 prescriptions, here are the top five errors tied to generics:
- Dosage confusion - A patient gets 10mg instead of 5mg because the label says “10” and the pharmacist missed the decimal. Generic tablets often have different strengths than the original, and prescribers don’t always update the script.
- Strength mismatch - The script says “Lisinopril 20mg,” but the pharmacy dispenses a 10mg tablet and tells the patient to take two. No one checks if the patient can safely split pills.
- Dispensing form errors - A patient gets a capsule when they were supposed to get a tablet. Or worse - they get a delayed-release version instead of immediate-release. This changes how the drug works in the body.
- Wrong manufacturer substitution - The patient has had bad reactions to a specific generic brand before. The pharmacy doesn’t record that. They just grab the cheapest one off the shelf.
- Labeling mistakes - The bottle says “Take twice daily,” but the original script said “Take twice weekly.” This happened in a documented case where a patient overdosed on a generic antifungal. The label was printed wrong by the manufacturer, and no one caught it.
These aren’t theoretical. They’re happening in your local pharmacy right now.
How to Prevent These Errors
Prevention doesn’t mean hiring more staff or spending millions. It means using proven tools - and doing the basics right.
1. Use the 8 R’s Every Time
It’s simple. Before you hand over any pill, ask:
- Right patient - Double-check name and date of birth. Don’t assume.
- Right drug - Is this the exact generic version the doctor ordered? Check the label against the script.
- Right dose - Does the tablet strength match? Are you giving one pill or two?
- Right route - Is it oral? Topical? Not injectable?
- Right time - Once a day? At bedtime? With food?
- Right documentation - Did you log the change in the system? Did you note the manufacturer?
- Right reason - Why is this generic being used? Is there a clinical reason?
- Right response - Did the patient have issues with this drug before? Did they say they didn’t feel right on the last batch?
It takes 30 seconds. But it catches 60% of errors before they leave the counter.
2. Mandatory Counseling for First-Time Generics
When a patient gets a new generic - especially if it’s their first time on that drug - talk to them. Not just say, “Here’s your script.” Ask: “This is a different brand than before. Have you ever had trouble with this medicine?”
Studies show this catches 12-15% of potential errors. Patients notice differences. They just don’t always speak up. One woman told her pharmacist she felt “weird” after switching generics. Turns out, the new version had lactose - and she was undiagnosed with lactose intolerance. She’d been getting stomach cramps for months and thought it was her diet.
3. Update Your Drug Reference Tools
Don’t rely on free apps or outdated books. Use tools like Drug Facts and Comparisons or Epocrates. They show you not just the drug name, but the manufacturer, color, shape, and inactive ingredients. Update them every year. The cost? $150-$300. The risk of getting it wrong? A patient’s life.
4. Use Technology - But Don’t Rely on It
Bar code scanning (BCMA) cuts dispensing errors by half. Computerized prescribing (CPOE) cuts errors by nearly 50%. But here’s the catch: most community pharmacies in Australia still don’t use these. If you’re in a chain pharmacy, ask your manager to install them. If you’re independent, look into low-cost systems like Medisafe or PharmAssist. They integrate with your existing software and flag look-alike drugs.
And turn off unnecessary alerts. Too many pop-ups make pharmacists ignore them. Only keep alerts for high-risk drugs - like insulin, warfarin, or seizure meds.
What to Do When an Error Happens
Errors happen. Even the best pharmacies make them. The key isn’t avoiding them - it’s fixing them fast.
If you realize you dispensed the wrong generic:
- Call the patient immediately. Don’t wait for them to come back. Say: “We made a mistake. You got the wrong version of your medicine. Please stop taking it and call us.”
- Document everything. What was dispensed? What should have been? Who checked it? When? This isn’t for blame - it’s for learning.
- Report it internally. If your pharmacy has a safety system, log it. If not, start one. Track every near-miss. Patterns show up over time.
- Follow up in 48 hours. Ask: “How are you feeling?” Some reactions are delayed.
One pharmacist in Melbourne did this after giving a patient the wrong generic of metformin. The patient had nausea and dizziness. She called, apologized, and offered a free consultation. The patient didn’t sue. She thanked her. And now, that pharmacist trains new staff on the incident.
What Patients Can Do to Protect Themselves
Pharmacists aren’t the only ones who can stop these errors. Patients have power too.
- Ask: “Is this the same as my last bottle?” If it looks different, say so.
- Keep a list of which generic brand you’ve been on. Write down the color, shape, and imprint.
- Ask your pharmacist: “Has this been switched? Is it safe for me?”
- If you feel worse after a switch - even slightly - tell your doctor and pharmacist. Don’t assume it’s “just in your head.”
One man in Sydney noticed his new generic statin was making him muscle sore. He kept taking it for months. Then he Googled the imprint. Found out it was made by a company with a known recall for that batch. He switched back - and the pain went away.
The Future: Better Systems, Fewer Mistakes
The good news? Change is coming. The FDA’s 2022 GDUFA III rules now require manufacturers to notify pharmacies when they change generic formulations. Australia’s TGA is moving toward similar standards.
AI tools are being tested to predict which patients might react badly to certain generics based on their genetics, age, and other meds. Early pilots show a 22% drop in errors compared to standard systems.
But technology alone won’t fix this. It’s still people - pharmacists, doctors, patients - who catch the mistakes. The best system in the world won’t help if no one checks the label.
Generic drugs save billions. They’re safe. They’re necessary. But safety doesn’t come from cost savings. It comes from attention to detail. From asking questions. From listening. From not assuming.
Next time you hand someone a bottle of generic pills - pause. Look at it. Compare it. Talk to them. That one extra second might be the difference between a healthy day… and a hospital visit.
Are generic medications less safe than brand-name drugs?
No, generics are not less safe. They must meet the same FDA and TGA standards for effectiveness and purity as brand-name drugs. The difference isn’t in safety - it’s in appearance, fillers, and manufacturer consistency. Most patients never have an issue. But for some - especially those on multiple meds or with sensitivities - switching generics can cause unexpected reactions. That’s why tracking and communication matter.
Why do generic pills look different each time I refill?
Different manufacturers make the same generic drug. Each one uses different dyes, shapes, and sizes to distinguish their product. A blue 10mg lisinopril from one company might be white and oval from another. This isn’t a mistake - it’s normal. But if you’re used to one version and suddenly get another, it’s worth asking your pharmacist: “Is this the same medicine?”
Can I ask my pharmacist to always give me the same generic brand?
Yes. You can ask for a specific manufacturer by name. Some pharmacies will accommodate this, especially if you’ve had a reaction before. You may need to pay a bit more if that brand isn’t the cheapest option. But your health comes first. Write down the brand name, color, and imprint on your prescription list and bring it in each time.
Do pharmacists get training on generic medication errors?
Basic training is required for licensing, but ongoing, specific training on generic-related errors isn’t mandatory in most places. Many pharmacists learn through experience or peer sharing. The best pharmacies run monthly safety huddles where staff discuss near-misses. If yours doesn’t, ask for it. It’s one of the most effective ways to prevent errors.
How can I tell if my pharmacy is using good safety practices?
Look for these signs: Do they scan barcodes before dispensing? Do they ask you about side effects when you pick up a new generic? Do they have a quiet space for counseling? Do they offer to call your doctor if something looks off? If you’re not sure, ask: “Do you have a system to catch generic mix-ups?” A pharmacy that takes this seriously will have a clear answer.
Next Steps for Pharmacists and Patients
For pharmacists: Start today. Pick one thing to improve. Maybe it’s updating your drug database. Maybe it’s adding a checklist for first-time generics. Maybe it’s asking every patient: “Has this changed since your last fill?” One small step, repeated daily, prevents more errors than any expensive system.
For patients: Don’t stay silent. If your pills look different, ask. If you feel off after a switch, speak up. Your voice is the last line of defense.
Medication safety isn’t about perfection. It’s about awareness. And in a world full of generics, awareness is the only thing that can’t be bought - only practiced.

Joy Aniekwe
November 30, 2025 AT 01:24Oh wow, a whole essay on how generics can kill you if you blink wrong? And the pharmacist is just sitting there, sipping their overpriced oat milk latte, hoping the patient doesn't notice the pill changed from a blue oval to a white circle? Brilliant. I'm sure the FDA's 80-125% absorption range is just a cozy little suggestion, like 'please don't set your house on fire.' I'll be sure to carry a color-coded pill chart and a vibrating alarm that screams 'THIS ISN'T THE SAME BLUE PILL YOU GOT LAST MONTH!' next time I refill. Because clearly, my life depends on remembering which generic manufacturer hates me today.
Latika Gupta
December 1, 2025 AT 13:29I took a generic blood pressure med last year. The pill looked different. I didn’t say anything. I felt tired for weeks. Then I read the label again - the imprint was ‘L 20’ instead of ‘L 10’. I didn’t know you could split pills. I took two. My heart felt like it was trying to escape my chest. I didn’t tell anyone. I just switched back to brand. No one asked. No one cares.
Sullivan Lauer
December 2, 2025 AT 10:59Let me tell you - this is the single most important public health conversation we’re NOT having. I’ve worked in pharmacy for 22 years, and I’ve seen people end up in the ER because they got a generic version with a different filler - and no one told them. I’ve had patients cry because they thought their anxiety was getting worse - turns out, the new generic had dextrose, and they had undiagnosed diabetes. This isn’t about cost. It’s about dignity. It’s about trust. We treat patients like they’re just numbers on a screen, but every pill is a promise. And when that promise breaks - because a label was misprinted or a database wasn’t updated - someone’s life gets flipped upside down. We need mandatory patient counseling for every first-time generic switch. We need barcodes. We need training. We need to stop pretending this is just ‘business as usual.’ The system is broken - and we’re the ones holding the scissors.
Sohini Majumder
December 4, 2025 AT 01:04Matthew Higgins
December 5, 2025 AT 06:42Man, I used to work at a chain pharmacy in Ohio. We’d get these shipments from six different generic makers for the same drug - same name, same dosage, but one was pink, one was blue, one was shaped like a tiny coffin. One guy came in screaming because his ‘prozac’ was now a little white oval instead of a blue capsule. He said his depression came back overnight. We checked the database - it was the same drug, same manufacturer code, just a different batch. We apologized, swapped it back, and gave him a free coffee. He cried. We all did. Turns out, people don’t just take pills - they attach meaning to them. The color, the shape, the way it feels in their hand - it’s part of their routine. When that changes, it’s not just chemistry. It’s identity. And we don’t talk about that enough.
Mary Kate Powers
December 6, 2025 AT 22:56Thank you for writing this. I’ve been a nurse for 18 years, and I’ve seen too many patients confused by generic switches. One elderly lady thought her new ‘blood pressure pill’ was a vitamin because it was yellow and small. She took it with her morning tea instead of her usual evening dose - and ended up with a stroke. We didn’t catch it until it was too late. Please, if you’re on generics: write down the color, shape, and imprint on your phone. Take a picture of the bottle. Ask your pharmacist: ‘Is this the same as last time?’ And if you feel off - even a little - speak up. Your voice matters more than you know. You’re not being difficult. You’re being smart.
Steven Howell
December 7, 2025 AT 03:47It is imperative to underscore that the regulatory frameworks governing generic pharmaceuticals in both the United States and Australia are robust and grounded in rigorous bioequivalence standards. The variance in physical characteristics - including color, shape, and excipient composition - is neither a defect nor a regulatory failure, but rather an inherent consequence of competitive market dynamics. The primary locus of error lies not in the pharmacological equivalence of the active ingredient, but in the procedural inadequacies of dispensing protocols and patient communication. It is therefore incumbent upon healthcare practitioners to implement standardized verification protocols, including but not limited to: cross-referencing manufacturer identifiers, utilizing updated pharmaceutical databases, and engaging in deliberate patient counseling. The solution is not to restrict generic substitution, but to elevate the quality of professional practice.
Brandy Johnson
December 7, 2025 AT 13:41Let’s be honest - this is what happens when you let foreign manufacturers cut corners to save a buck. The FDA’s 80-125% range is a joke. We’re letting China, India, and Mexico produce our life-saving medications with no oversight, and now people are dying because some pharmacist didn’t notice a pill changed from blue to white? We need a national registry of generic manufacturers. We need mandatory labeling in English with the country of origin. We need to stop outsourcing our health to countries that don’t even have clean water. This isn’t ‘affordability’ - it’s national security. And until we treat medication like we treat our borders, we’re just asking for more tragedies.
Peter Axelberg
December 8, 2025 AT 04:40I’ve been in this game since the 90s. Back then, we used paper books with faded photos of pills. Now we’ve got apps, barcodes, AI - and yet, I still see the same mistakes. Why? Because people are tired. Pharmacists are overworked. Patients are distracted. The system isn’t broken - it’s just exhausted. I don’t need more tech. I need more time. One extra minute with a patient. One extra check. One question: ‘Does this feel right to you?’ That’s the magic bullet. I had a guy come in last week with a new generic metformin. He said, ‘It tastes weird.’ I looked it up - new batch, different coating. He’d been getting stomach cramps for two months. We swapped it back. He thanked me. No lawsuit. No drama. Just a minute of listening. That’s all it takes. We just forgot how to do it.