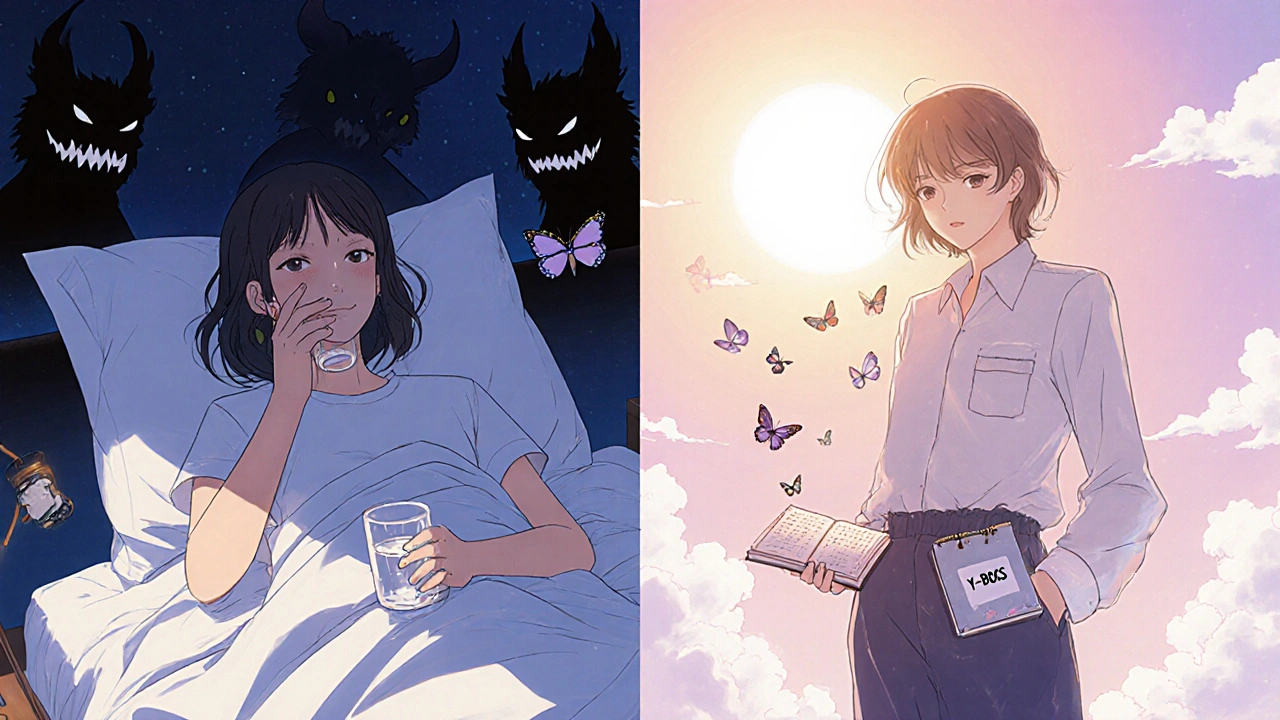
When OCD symptoms feel overwhelming, medication can be a lifeline. But not all meds work the same way, and dosing isn’t one-size-fits-all. If you’re trying to understand what actually works-beyond the hype-you need clear, real-world info on SSRIs and clomipramine, including how much to take, when to expect results, and why side effects matter more than you think.
SSRIs Are the First Step, But Not Because They’re Magic
Selective serotonin reuptake inhibitors (SSRIs) are the go-to starting point for OCD treatment. That’s not because they’re perfect-it’s because they’re the least bad option. The American Psychiatric Association recommends them as first-line because they’re safer than older drugs like clomipramine, with fewer risks to your heart, liver, or daily function.
But here’s the catch: the doses used for OCD are way higher than what’s prescribed for depression. If you’ve tried an SSRI for anxiety and it didn’t help, you probably weren’t on a high enough dose. For OCD, you need to push past the depression dose and aim for the OCD dose. That means:
- Fluoxetine (Prozac): 40-60 mg/day
- Sertraline (Zoloft): 200-300 mg/day
- Fluvoxamine (Luvox): 200-300 mg/day
- Paroxetine (Paxil): 40-60 mg/day
These aren’t suggestions-they’re clinical targets. Studies show you need at least six weeks at one of these doses to even begin seeing results. Most people don’t notice real change until week 8-12. If you quit after four weeks because you felt worse, you’re not failing-you’re just early.
Starting low is key. Doctors usually begin with 25 mg of sertraline or 12.5 mg of fluvoxamine. Why? Because in the first 1-2 weeks, OCD symptoms can spike. Up to 37% of patients report increased anxiety, intrusive thoughts, or even panic attacks during this window. It’s not the medication failing-it’s your brain adjusting. Most people who stick through it see improvement by week 4. If you’re scared, talk to your doctor about starting at half-dose and going slower.
Clomipramine: The Old Warrior with a Reputation
Clomipramine was the first drug ever approved by the FDA specifically for OCD-in 1989. It’s a tricyclic antidepressant, older than SSRIs, and it works differently. It doesn’t just boost serotonin; it also affects norepinephrine. That’s why it’s more powerful-but also more punishing.
For adults, the standard starting dose is 25 mg per day. That’s tiny. Then, every 4-7 days, your doctor may bump it up by 25 mg. The goal? 100-250 mg per day. Most people need at least 150 mg to feel a difference. In kids 10 and older, dosing is based on weight: 1-3 mg per kg, max 200-250 mg depending on the guideline.
Here’s what you won’t hear from every doctor: clomipramine works better for contamination and cleaning rituals. If your OCD is all about germs, washing, or fear of touching things, this drug has a stronger track record than SSRIs in some studies. A meta-analysis showed it improved OCD symptoms by 37% in children and teens-better than sertraline or fluoxetine.
But the trade-off is real. Three to five times more people quit clomipramine because of side effects. Dry mouth so bad you need five glasses of water an hour. Weight gain of 15-25 pounds in six months. Constant drowsiness. Blurred vision. Constipation. Heart rhythm changes. QTc prolongation is a real risk when doses go over 150 mg/day, which is why doctors order ECGs before and during treatment.
That’s why it’s not first-line. It’s reserved for when SSRIs fail-or used as an add-on. About 22% of people with treatment-resistant OCD end up on clomipramine. And for those who stick with it, the payoff can be life-changing. One Reddit user wrote: “After five failed SSRIs, clomipramine at 175 mg finally stopped my checking rituals. But the drowsiness? I switched back to sertraline.” That’s the story for a lot of people.
Dosing Isn’t Just About Numbers-It’s About Timing
When you take the pill matters as much as how much you take. Clomipramine is heavily sedating. That’s why it’s almost always taken at bedtime. If your dose is 150 mg, your doctor might split it: 100 mg at night, 50 mg in the morning. This helps with sleep and reduces daytime grogginess.
SSRIs are usually taken in the morning. Why? Because they can cause insomnia or jitteriness, especially early on. Taking sertraline at night might wreck your sleep. But if you’re on a high dose and feel nauseous or anxious during the day, some people find taking it at night helps.
And don’t forget: you need blood tests for clomipramine. Therapeutic levels are between 220-350 ng/mL for clomipramine and 379 ng/mL for its metabolite, desmethylclomipramine. If you’re on 200 mg and not improving, your doctor should check your blood levels. You might be metabolizing it too fast-or too slow.

How Do You Know If It’s Working?
It’s not about feeling “better.” It’s about measurable change. Clinicians use the Yale-Brown Obsessive Compulsive Scale (Y-BOCS). A 25-35% drop in score is considered a good response. That means if your obsessions used to take 4 hours a day and you did 10 compulsions, now you’re down to 2.5 hours and 6-7 rituals. That’s success.
Most people don’t realize how slow this is. You’re not going to wake up one day and feel “cured.” You’ll notice small wins: you didn’t wash your hands after touching the doorknob. You left the stove on and didn’t go back to check. You sat through a 10-minute thought without trying to neutralize it.
Track it. Use a journal. Write down your Y-BOCS score every 2-4 weeks. If nothing changes after 12 weeks at the right dose, it’s time to talk about switching or adding something.
Why Do People Quit? And What Happens When They Do?
SSRIs have a 15-18% discontinuation rate due to side effects. Clomipramine? 28%. That’s a huge gap. The most common reasons? Dry mouth, weight gain, drowsiness, sexual dysfunction, and feeling emotionally numb.
But here’s the thing: people who quit too soon never find out if it would’ve worked. A 2019 NIMH study found that 89% of those who stopped because of early anxiety saw their symptoms improve if they kept going. The first two weeks are the hardest. That’s when your brain is rewiring. If you give up then, you’re quitting before the medicine even has a chance.
And if you do stop? Don’t quit cold turkey. Taper slowly. Abruptly stopping SSRIs can cause dizziness, brain zaps, nausea, and rebound anxiety. Clomipramine withdrawal can be even worse-seizures, hallucinations, extreme agitation. Always work with your doctor to come off slowly.
The Future: What’s Next Beyond SSRIs and Clomipramine?
There’s new stuff coming. In March 2023, the FDA gave Breakthrough Therapy status to SEP-363856, a new serotonin modulator. In a phase 2 trial, it helped 45% of people with treatment-resistant OCD at just 50 mg/day. That’s promising.
Psilocybin-yes, the compound in magic mushrooms-is being tested in phase 3 trials with SSRIs. Early results show 60% remission at six months, compared to 35% with SSRIs alone. It’s not available yet, but it’s real.
As for clomipramine, researchers are testing a skin patch to deliver it slowly. Early data shows the same effectiveness at 150 mg patch vs. 200 mg pill-with 40% fewer side effects. That could change everything.
For now, though, SSRIs and clomipramine are still the backbone. The choice isn’t about which is “better.” It’s about which is tolerable for you.
What to Do Next
- If you’re new to OCD meds: start with an SSRI. Pick one your doctor recommends. Start low. Go slow.
- If you’ve tried one SSRI and failed: try a different one. Not all SSRIs work the same for OCD.
- If you’ve tried two SSRIs for 12 weeks each and still struggle: ask about clomipramine. Don’t wait until you’re desperate.
- If you’re on clomipramine and side effects are unbearable: talk about lowering the dose or switching to an SSRI + low-dose clomipramine combo (25-75 mg). Many people find this works better than either alone.
- Always get a baseline ECG before starting clomipramine. Always get blood levels checked if you’re not responding.
- Track your symptoms. Use the Y-BOCS scale. Numbers don’t lie.
OCD medication isn’t a quick fix. It’s a marathon with a lot of stops along the way. But for thousands of people, it’s the only thing that brought them back from the edge.
How long does it take for OCD medication to work?
Most people need 8 to 12 weeks to see real improvement. You should be on a full therapeutic dose for at least six weeks before deciding if it’s working. Don’t give up before week 8-early worsening is common and usually temporary.
Is clomipramine stronger than SSRIs for OCD?
In head-to-head trials, clomipramine and SSRIs are equally effective for adults. But in children and teens, clomipramine shows slightly better results-especially for contamination fears. However, it causes 3-5 times more side effects, so SSRIs are still first-line.
Can I take clomipramine and an SSRI together?
Yes-this is called augmentation. Many doctors add a low dose of clomipramine (25-75 mg/day) to an SSRI if the SSRI alone isn’t enough. This approach works for 35-40% of people who didn’t respond to SSRIs alone. But it requires close monitoring due to increased risk of serotonin syndrome.
Why do SSRIs for OCD need higher doses than for depression?
OCD is more resistant to serotonin modulation than depression. Studies show that doses effective for depression (e.g., 20 mg of sertraline) rarely help OCD. You need to push higher-often 2-3 times the depression dose-to trigger the brain changes needed to reduce obsessions and compulsions.
What if my OCD meds stop working after months?
Tolerance can happen, but it’s rare. More often, life stress, lack of therapy, or poor sleep undermines progress. Before changing meds, review your therapy (CBT/ERP), sleep, and stress levels. If those are stable and symptoms are returning, talk to your doctor about switching or adding an augmentation agent like low-dose clomipramine.
Are there any natural alternatives to OCD medication?
No natural supplement has been proven to replace SSRIs or clomipramine for moderate to severe OCD. Some people report mild help from NAC (N-acetylcysteine) or inositol, but these aren’t substitutes. Evidence-based treatment still requires FDA-approved medication combined with exposure and response prevention (ERP) therapy.
Troubleshooting Common Issues
- Worse anxiety at first? Stick with it. 89% of people improve if they continue. Talk to your doctor about starting at half-dose.
- Weight gain? Clomipramine causes this more than SSRIs. Ask about switching or adding metformin (off-label) if it’s significant.
- Sexual side effects? Common with SSRIs. Try lowering the dose slightly, switching to bupropion (off-label), or adding a low-dose phosphodiesterase inhibitor-only under medical supervision.
- Can’t sleep on SSRIs? Move the dose to morning. If that doesn’t help, try a low-dose trazodone at night (not for OCD, just for sleep).
- Clomipramine making me dizzy? Check your blood pressure. It can cause orthostatic hypotension. Stand up slowly. Avoid alcohol.


Jesús Vásquez pino
November 25, 2025 AT 21:16SSRIs at OCD doses are basically just serotonin sledgehammers and you gotta ride the wave or get crushed. I went from 50mg sertraline to 250mg over 3 months and yeah, I felt like a zombie for 6 weeks - but then I stopped checking if my front door was locked 17 times a night. Worth it. Don’t quit at week 4.
hannah mitchell
November 26, 2025 AT 13:54I appreciate how real this is. No sugarcoating. I was on clomipramine for 8 months and the dry mouth was so bad I kept a water bottle taped to my desk. But I finally slept through the night for the first time in 5 years. Side effects suck, but so does living in your head all day.
stephen riyo
November 27, 2025 AT 22:56Wait, so… you’re saying if you don’t hit 200mg+ on sertraline, you’re basically just taking a placebo for OCD? That’s wild. I tried 100mg for 6 weeks and quit because I felt ‘weird’… now I’m realizing I didn’t even try. Damn.
Jaspreet Kaur
November 28, 2025 AT 23:11Medication is just one tool in the fire. The real work is ERP. I was on 300mg fluvoxamine and still stuck in loops until I started doing exposure daily. The pill quieted the noise enough to hear myself think. But it didn’t fix me. I did.
Gina Banh
November 30, 2025 AT 16:25Clomipramine isn’t ‘stronger’ - it’s just less selective. It hits every receptor like a drunk guy at a party. That’s why it works for contamination OCD - it’s brute force serotonin. But if you’re not ready for the side effect buffet, don’t touch it. And yes, blood levels matter. Stop guessing.
Bethany Buckley
December 2, 2025 AT 15:59It’s fascinating how the pharmacokinetics of clomipramine’s metabolite, desmethylclomipramine, exhibits a higher affinity for SERT than the parent compound - yet clinicians still treat it as a monolithic agent. The therapeutic window is narrow, and the CYP2D6 polymorphism variance is grossly under-monitored. 🤔💊
Stephanie Deschenes
December 3, 2025 AT 19:06To anyone reading this and feeling overwhelmed: you’re not broken. You’re not failing. This is hard. I was on 5 different SSRIs over 3 years. I cried every time I skipped a dose. But when I finally hit the right combo - sertraline 200mg + 50mg clomipramine at night - I could breathe again. It’s not a cure, but it’s peace. You deserve that.
Cynthia Boen
December 3, 2025 AT 21:05Why are we still using 1989 drugs? This is 2024. We have ketamine, psilocybin, and neurostimulation - but no one talks about it because Big Pharma loves selling SSRIs for life. This whole post feels like a pharmaceutical pamphlet with footnotes.