Most people with fatty liver don’t feel sick. No pain. No jaundice. No warning signs. That’s why NAFLD sneaks up on so many - it’s silent until the damage is done. Around 1 in 4 adults worldwide have some form of fatty liver disease, and in Australia, that number is climbing fast. But not all fatty liver is the same. The difference between simple fatty liver (NAFL) and its more dangerous cousin (NASH) can mean the difference between a routine check-up and a life-altering diagnosis.
What’s the Real Difference Between NAFL and NASH?
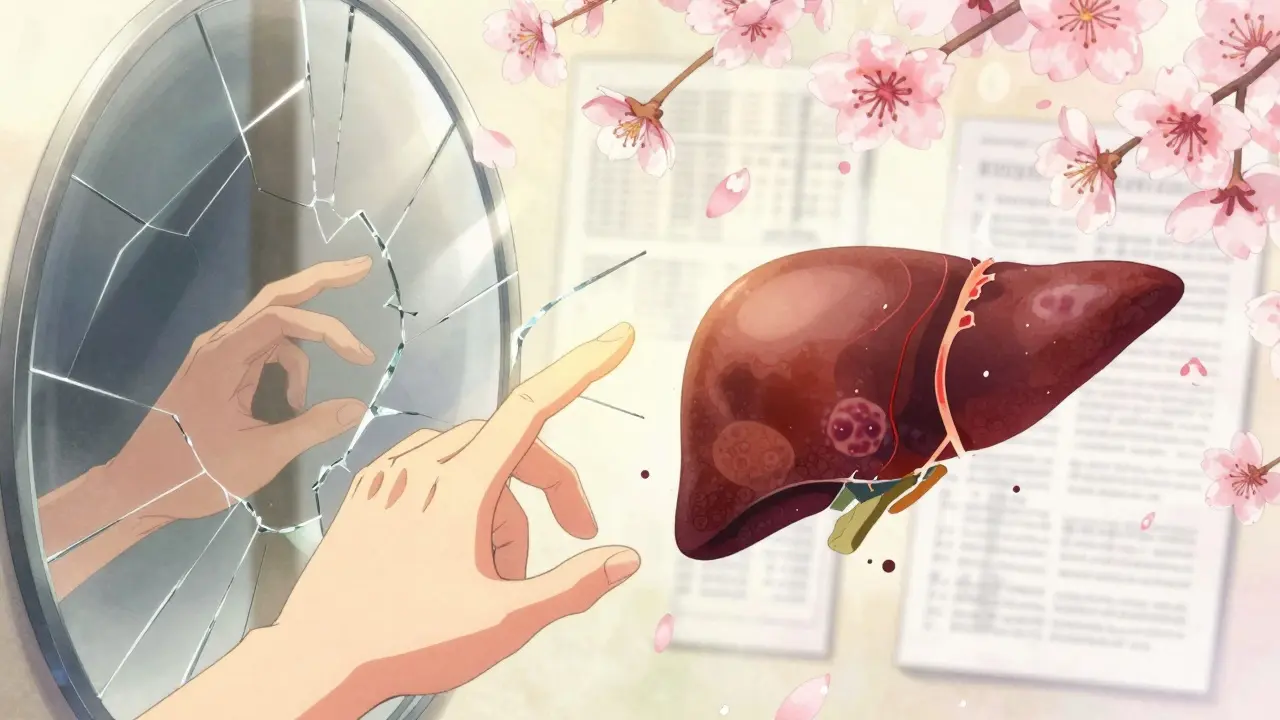
Think of NAFLD as an umbrella. Under it are two main conditions: Non-Alcoholic Fatty Liver (NAFL) and Non-Alcoholic Steatohepatitis (NASH). Both start the same way - with too much fat building up in the liver. That’s it. No inflammation. No cell damage. Just fat. If your liver has 5% or more fat and nothing else, you have NAFL. It’s common. It’s often harmless. Many people live with it for decades without problems. NASH is the next step. Same fat buildup - but now there’s inflammation. Liver cells are swelling and dying. This is called ballooning. And when that happens, your liver starts trying to heal itself by forming scar tissue - fibrosis. That’s the real danger. Fibrosis doesn’t reverse easily. Once it starts, it can creep toward cirrhosis, liver failure, or even cancer. The 2023 guidelines from the American Association for the Study of Liver Diseases (AASLD) and European Association for the Study of the Liver (EASL) have updated the names: NAFL is now called MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease), and NASH is MASH (Metabolic Dysfunction-Associated Steatohepatitis). The change isn’t just semantics. It shifts focus from what you don’t do (drink alcohol) to what you do have - metabolic problems like obesity, high blood sugar, and high triglycerides. That’s the real root cause.How Do You Know If You Have NASH - Not Just Fatty Liver?
Blood tests won’t tell you for sure. Your ALT and AST levels might be slightly high - say, 60 or 70 instead of the normal 40 - but they can also be normal even with serious damage. Ultrasound can spot fat in the liver, but it can’t tell if there’s inflammation or scarring. That’s why most people with NASH are diagnosed by accident - during a routine scan for something else. The only way to confirm NASH is a liver biopsy. It’s invasive. It’s not for everyone. But if you’re at high risk - you’re overweight, have type 2 diabetes, or your FIB-4 score is over 1.3 - your doctor might recommend it. The FIB-4 score uses your age, platelet count, ALT, and AST to estimate fibrosis risk. A score above 2.67 means you’re likely in stage 3 or 4 fibrosis. That’s serious. Newer tools like FibroScan are becoming more common. It’s a painless ultrasound that measures liver stiffness. If the reading is above 7.1 kPa, it suggests fibrosis. Above 10 kPa? High chance of advanced scarring. These tools are changing how we screen - but they’re not perfect. FibroScan can miss early damage. Biopsy still wins when you need certainty.Fibrosis Is the Real Killer - Not the Fat
Here’s what most people don’t realize: it’s not the fat that kills you. It’s the scar tissue. Fibrosis is staged from 0 to 4:- Stage 0: No scarring
- Stage 1: Minor scarring around veins
- Stage 2: Scarring spreading
- Stage 3: Bridging fibrosis - scars start connecting
- Stage 4: Cirrhosis - the liver is hardened and failing
Who’s at Risk? The Hidden Triggers
You don’t have to be obese to get NASH - but most people who do are. Around 70% to 90% of NASH patients have a BMI over 30. But here’s the twist: 20% of NASH patients are normal weight. They have what’s called "lean NASH." It’s rare, but it happens. Their metabolic health is broken - insulin resistance, high triglycerides, low HDL - even if they look fine. Type 2 diabetes? That’s the biggest red flag. Half to 70% of NASH patients have it. High blood pressure? That’s in 60% to 75%. Obstructive sleep apnea? It’s linked in 30% to 50%. These aren’t random. They’re part of the same metabolic mess - insulin resistance, belly fat, inflammation. The scary part? Most people don’t know they’re at risk until they’re diagnosed with stage 2 fibrosis. One Reddit user, LiverWarrior2022, had ALT levels over 60 for three years - no symptoms - then found out he had stage 2 scarring. That’s not unusual. A 2022 survey found 41% of patients waited 6 to 24 months between abnormal blood tests and seeing a specialist.Can You Reverse It?
Yes. But only if you act early. Weight loss is the most powerful treatment we have. Losing 7% to 10% of your body weight can reverse NASH in most people. A 2023 registry study showed that 90% of patients who hit that target saw their NASH turn back into simple fatty liver. Fibrosis improved in 85%. It’s not about crash diets. It’s about sustainable change: cutting sugar, reducing processed carbs, moving daily, sleeping better. A 2022 Lancet study showed that a 1% annual rise in obesity leads to 4.7 million more NASH cases in the U.S. alone. We’re in a public health crisis. There’s also new hope. In March 2023, the FDA approved resmetirom (Rezdiffra) - the first drug specifically for NASH patients with moderate to advanced fibrosis. In trials, it improved fibrosis in 26% of patients. That’s not a cure. But it’s a start. Over 30 drugs are in phase 3 trials. For the first time, we’re not just telling people to lose weight - we’re giving them real tools.
What Should You Do If You’re Diagnosed?
If you’ve been told you have fatty liver:- Don’t panic. Most cases are still NAFL/MASLD.
- Get your FIB-4 score calculated. Ask your doctor for your ALT, AST, platelet count, and age.
- If your score is over 1.3, ask about FibroScan.
- If you have diabetes, high blood pressure, or obesity - treat those first. Medications like GLP-1 agonists (semaglutide, tirzepatide) aren’t approved for NASH yet - but they help with weight and insulin resistance, which directly help the liver.
- Get moving. 150 minutes of brisk walking a week cuts fibrosis risk by nearly half.
- Stop drinking alcohol. Even if you’re "non-alcoholic," alcohol adds fuel to the fire.
The Bottom Line
NAFLD isn’t just "a little fatty liver." It’s a spectrum - and NASH is the point where things get dangerous. The fat alone isn’t the enemy. It’s the inflammation and fibrosis that turn it into a silent killer. The good news? You can stop it. You can reverse it - if you catch it early. The tools are here. The knowledge is here. What’s missing is awareness. If you’re overweight, diabetic, or just have abnormal liver tests - don’t ignore it. Get the right tests. Ask about fibrosis. Take action. Your liver doesn’t scream. But it will break - if you don’t listen.Is NAFLD the same as NASH?
No. NAFLD is the umbrella term for all fatty liver conditions not caused by alcohol. NASH is a more serious subtype of NAFLD that includes inflammation and liver cell damage. Think of NAFL as fat in the liver with no harm done. NASH means fat plus active damage - which can lead to scarring and cirrhosis.
Can you have NASH without being overweight?
Yes. About 20% of NASH patients have a normal BMI. This is called "lean NASH." It’s linked to insulin resistance, high triglycerides, low HDL, and genetic factors - even if you don’t look overweight. Metabolic health matters more than body size.
How is NASH diagnosed?
Blood tests and ultrasound can suggest fatty liver, but only a liver biopsy can confirm NASH. Non-invasive tools like FibroScan and FIB-4 scores help identify who needs a biopsy. FibroScan measures liver stiffness - high readings suggest fibrosis. FIB-4 uses age, platelets, ALT, and AST to estimate risk. A FIB-4 score over 1.3 raises concern; over 2.67 means advanced fibrosis is likely.
Can NASH be reversed?
Yes - if caught early. Losing 7% to 10% of body weight can reverse NASH in most people and improve fibrosis in 85%. Lifestyle changes - diet, exercise, sleep - are the most effective treatments. New drugs like resmetirom (Rezdiffra) are now approved for patients with moderate to advanced fibrosis, offering another tool.
What’s the difference between MASLD and NAFLD?
MASLD is the new name for NAFLD, introduced in 2023. The change removes the word "non-alcoholic" to reduce stigma and better reflects the real cause: metabolic dysfunction. MASLD diagnosis requires at least one metabolic risk factor - like obesity, diabetes, high blood pressure, or abnormal cholesterol - regardless of alcohol use. NASH is now called MASH.
When should I see a specialist?
See a hepatologist if your FIB-4 score is over 1.3, FibroScan shows liver stiffness above 7.1 kPa, you have type 2 diabetes with elevated liver enzymes, or you’ve been told you have fibrosis. Early specialist care improves outcomes. Waiting until symptoms appear - like fatigue or abdominal pain - often means the damage is already advanced.

Sazzy De
January 31, 2026 AT 20:08Don’t wait until you’re tired all the time.
Gaurav Meena
January 31, 2026 AT 20:58kate jones
February 1, 2026 AT 07:38Natasha Plebani
February 2, 2026 AT 03:13Rob Webber
February 2, 2026 AT 20:08calanha nevin
February 4, 2026 AT 06:43Lisa McCluskey
February 5, 2026 AT 08:18owori patrick
February 5, 2026 AT 13:15Claire Wiltshire
February 6, 2026 AT 14:02April Allen
February 7, 2026 AT 15:23Donna Fleetwood
February 8, 2026 AT 22:11Melissa Cogswell
February 10, 2026 AT 21:05Shubham Dixit
February 11, 2026 AT 00:53KATHRYN JOHNSON
February 11, 2026 AT 11:10