When someone has type 2 diabetes and struggles with obesity, medication alone often isn’t enough. Many people spend years trying diet, exercise, and pills-only to see their blood sugar creep back up. But there’s another path: metabolic surgery. It’s not just about losing weight. For many, it’s the only treatment that actually reverses diabetes.
What metabolic surgery actually does
Metabolic surgery isn’t one procedure. It’s a group of operations that change how your stomach and intestines work. The most common are gastric bypass, sleeve gastrectomy, and duodenal switch. These aren’t cosmetic fixes. They rewire your body’s metabolism. After surgery, hormones that control hunger and blood sugar change almost immediately. Many patients see their blood sugar drop within days-even before they’ve lost much weight. This isn’t theory. In the Swedish Obese Subjects study, 30% of patients who had metabolic surgery were still in diabetes remission 15 years later. Only 7% of those who stuck with medication alone reached that point. That’s a four-fold difference. And it’s not just about the numbers. People report feeling more energy, needing fewer pills, and no longer fearing diabetic complications like nerve damage or kidney failure.Which surgery works best?
Not all surgeries are the same. The type you get matters a lot.- Gastric bypass (RYGB): This is the gold standard. At one year, 42% of patients are in full diabetes remission. At five years, it’s still 29%. Weight loss averages 27% of total body weight.
- Sleeve gastrectomy: More popular now because it’s simpler and safer. Remission rates are lower: 37% at one year, dropping to 23% by year five. But weight loss is still strong-around 25% of body weight.
- Duodenal switch: Highest remission rate-up to 95% in the first year. But it’s more complex, with higher risk of nutrient deficiencies. Used mostly for people with very high BMI.
- Gastric banding: Once common, now rarely used. Only 57% remission at one year, and it often slips over time.
Who sees the best results?
Not everyone responds the same. Success depends on more than just your weight.- Insulin use: If you’re still taking insulin before surgery, your chances of remission drop sharply. Patients not on insulin have over 50% remission rates. Insulin users? Closer to 20-30%.
- BMI range: You don’t need to be severely obese. Studies show people with BMI as low as 24-30 can still get 93% remission after gastric bypass. The American Diabetes Association now recommends surgery for those with BMI 30-34.9 if diabetes isn’t controlled by meds.
- How long you’ve had diabetes: The sooner you act, the better. If you’ve had diabetes for less than five years, your pancreas still has enough function to recover. After ten years, beta cells are often too worn out.
- Age: Younger patients tend to do better. But even people in their 60s can achieve remission if they’re otherwise healthy.
What happens after surgery?
Surgery isn’t the finish line-it’s the start of a new routine. You’ll need lifelong follow-up. Nutrient deficiencies are real. Iron, vitamin B12, calcium, and vitamin D levels drop without careful monitoring. Many patients need supplements for life. Bone fractures and anemia are more common after surgery than in non-surgical groups. Weight regain can happen. About 1 in 5 patients gain back some weight after five years. That’s why remission rates drop over time. But even with regain, most people still have better blood sugar control than before surgery. They use fewer drugs. Their A1C stays lower. Their risk of heart disease and kidney damage drops. Dr. David Arterburn from Kaiser Permanente warns: "The decline in remission over time is real. It’s not a cure. It’s a powerful tool that needs ongoing care."Why isn’t everyone getting this done?
The evidence is strong. The American Diabetes Association, the International Diabetes Federation, and the NIH all endorse metabolic surgery. Yet in the U.S., only 1-2% of eligible patients get it. Why?- Insurance won’t cover it: Many plans only approve surgery for BMI 35 or higher-even though guidelines now say 30+ qualifies if diabetes is uncontrolled.
- Doctors don’t recommend it: Many primary care providers still think surgery is a last resort. They don’t know the data.
- Patient fear: People hear "surgery" and think "death risk." But the death rate for gastric bypass is lower than for gallbladder removal. Complication rates have dropped by 70% since the 1990s.
- Access: You need a specialized center with a team: surgeon, dietitian, psychologist, endocrinologist. These aren’t available everywhere.

The bigger picture: It’s not just about weight
Metabolic surgery changes your body’s biology. It’s not just about shrinking your stomach. It’s about resetting your hormones. After bypass, your gut releases more GLP-1 and PYY-hormones that make you feel full and help your pancreas produce insulin. That’s why blood sugar drops so fast. Dr. Francesco Rubino, a leading expert in London, says: "Diabetes resolves before you lose much weight. That proves it’s not just about calories. It’s about how your body communicates with itself." This is why non-surgical options like very low-calorie diets (like the DiRECT trial) can work-but only for a year or two. Surgery creates lasting changes. Even when people gain back 10 pounds, their metabolism doesn’t revert.What’s next?
New procedures are coming. Endoscopic sleeve gastroplasty, gastric balloons, and aspiration therapy (like AspireAssist) are less invasive. They’re not as effective as bypass-but they’re options for people who aren’t ready for surgery. The RESET trial is testing metabolic surgery in patients with BMI 27-35. If it succeeds, eligibility could expand dramatically. Imagine a 40-year-old with prediabetes and BMI 31 getting surgery before they even develop full-blown diabetes. The future isn’t just about fixing obesity. It’s about preventing diabetes before it takes hold.Is it right for you?
Ask yourself:- Have you tried diet, exercise, and medications for at least six months?
- Are you still taking insulin or multiple diabetes pills?
- Is your A1C above 7.5% despite treatment?
- Do you have other obesity-related issues: sleep apnea, fatty liver, high blood pressure?
Can metabolic surgery cure type 2 diabetes?
Metabolic surgery doesn’t guarantee a permanent cure, but it’s the most effective treatment we have for long-term diabetes remission. About 30% of patients stay in remission 15 years after surgery. Many others see major improvements-even if they don’t meet the full remission criteria. Blood sugar stays lower, medications drop, and complications decrease.
How much weight do people lose after metabolic surgery?
On average, patients lose 25-30% of their total body weight within the first year. Gastric bypass patients typically lose more than those who get a sleeve gastrectomy. By five years, most keep off 20-25% of their original weight. That’s far more than what’s achieved with diet and exercise alone, which usually results in less than 5% weight loss over the same period.
Is metabolic surgery safe?
Yes, for most healthy adults. The risk of death within 30 days is less than 0.3%-lower than gallbladder surgery. Major complications like leaks or infections happen in fewer than 5% of cases. Long-term risks include nutrient deficiencies, which can be managed with supplements and regular blood tests. The biggest risk isn’t the surgery itself-it’s not doing anything at all when diabetes and obesity are getting worse.
Do I need to be overweight to qualify?
No. While surgery was once only for people with BMI 35+, guidelines now support it for those with BMI 30-34.9 if diabetes isn’t controlled with medication. Even patients with BMI under 30 have seen remission-especially after gastric bypass. The key factor isn’t just weight. It’s how long you’ve had diabetes, whether you’re on insulin, and how well your body still responds to insulin.
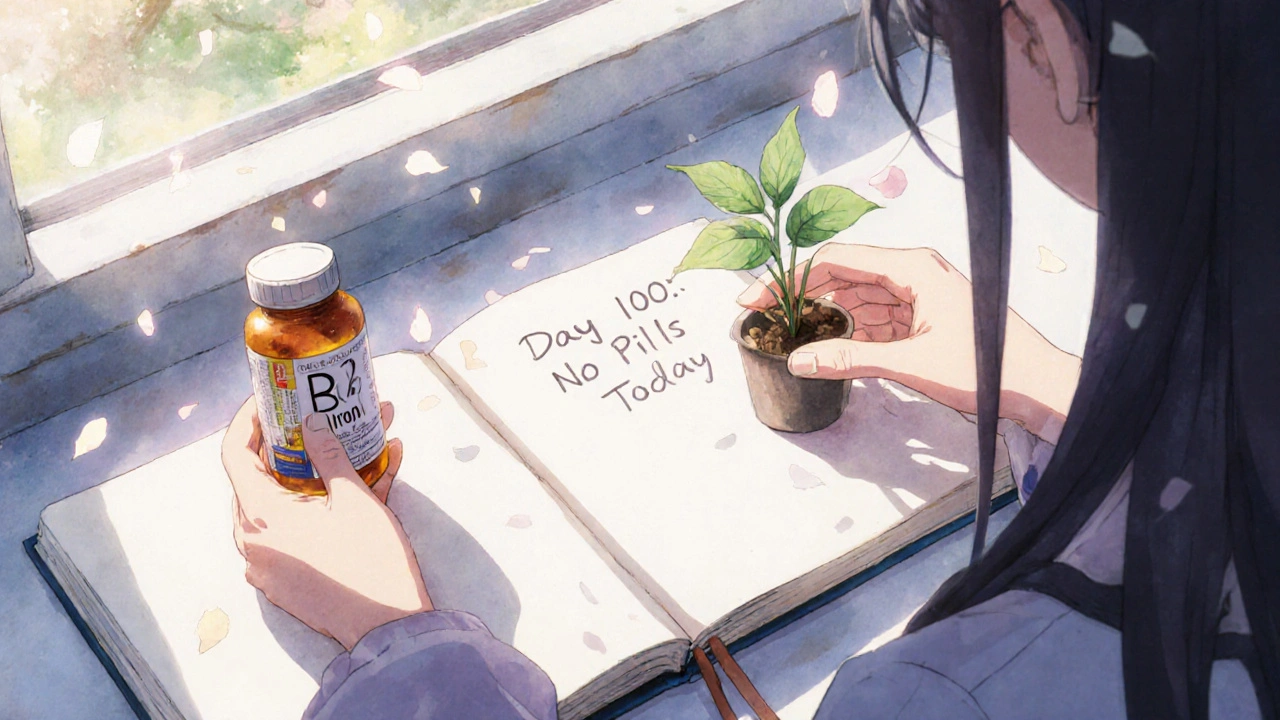
Will I need to take supplements forever?
Yes. After any metabolic surgery, your body absorbs fewer nutrients. You’ll need lifelong supplements: vitamin B12, iron, calcium, vitamin D, and often a multivitamin. Blood tests every 6-12 months are required. Skipping these can lead to anemia, nerve damage, or bone loss. It’s not optional-it’s part of the treatment.
Can I reverse diabetes without surgery?
Yes-but it’s harder and less durable. The DiRECT trial showed that a very low-calorie diet can lead to 46% remission at one year. But after five years, only about 15% stay in remission. Surgery gives you a much higher chance of lasting results. For people who’ve struggled for years, surgery offers a more reliable path to freedom from daily diabetes management.


Daniel McKnight
November 25, 2025 AT 08:16Man, I wish my PCP had told me this five years ago. I’ve been on metformin since 2019 and my A1C still hovers around 8.5. I thought surgery was for people who weigh 400 pounds - turns out I was the target demographic all along.
Now I’m researching surgeons. No more bandaids.
Jaylen Baker
November 26, 2025 AT 02:25Let me just say… this is the most hope I’ve felt in a decade. I’ve tried keto, intermittent fasting, Ozempic, you name it. Nothing stuck. But this? This feels like a real reset. Not a miracle. Not magic. Just biology, finally working the way it’s supposed to. I’m booking a consult next week. No more living in fear of amputations.
Thank you for sharing this.
Fiona Hoxhaj
November 26, 2025 AT 16:30How quaint. We’ve reduced the profound, systemic failure of modern metabolic medicine to a surgical procedure-reductive, almost bourgeois in its presumption that biology can be fixed with a scalpel and a multivitamin.
True healing requires ontological reorientation, not resection. The body is not a machine to be calibrated, but a symphony of entangled energies-your pancreas doesn’t ‘fail,’ it withdraws in protest against the capitalist diet-industrial complex.
Perhaps, before cutting, one should first question the moral architecture of the American food supply.
Merlin Maria
November 28, 2025 AT 08:46Incorrect. The 30% 15-year remission rate is misleading. You’re ignoring attrition bias. Many patients who relapse drop out of studies. Also, the DiRECT trial’s five-year data is more robust than you imply. And you completely omit the fact that GLP-1 agonists now rival surgical outcomes in controlled trials. This isn’t a cure-it’s a high-risk, high-cost gamble dressed as science.
Also, vitamin B12 deficiency isn’t ‘manageable’-it’s permanent neurological damage waiting to happen.
Nagamani Thaviti
November 29, 2025 AT 21:21Kamal Virk
November 30, 2025 AT 15:41It’s not that surgery is ineffective-it’s that the medical establishment is terrified of empowering patients. If people realize they can reverse diabetes without lifelong pharmaceutical dependency, the entire drug industry collapses. That’s why your doctor won’t mention it. That’s why insurance denies it. That’s why the ADA’s guidelines are watered down.
This isn’t medicine. It’s economics.
Elizabeth Grant
December 1, 2025 AT 23:17My cousin had the sleeve last year. She’s down 80 pounds, off all meds, and actually sleeps through the night now. I cried when she told me.
But the supplements? Oh man. She’s got a little pill organizer that looks like a pharmacy exploded in it. B12 shots every month, iron tabs, calcium chewables. It’s a lifestyle, not a quick fix.
But worth it? 100%.
Also, the post-op support group? Lifesaver. Find one.
angie leblanc
December 3, 2025 AT 13:57Did you know the FDA approved gastric bypass in 1991… right after the first GMO corn crops were planted? Coincidence? I think not.
They want you dependent on synthetic vitamins because the real nutrients are poisoned by glyphosate. That’s why you need supplements after surgery-your body’s trying to detox from corporate food.
Also, the ‘remission’ is just a placebo effect from being scared into eating salad. They don’t tell you that.
LaMaya Edmonds
December 3, 2025 AT 21:14Let’s be real-this is just the pharma-industrial complex’s new revenue stream. You think they want you cured? No. They want you on lifelong B12, calcium, and iron. That’s a $3,000/year recurring revenue model.
And don’t get me started on the ‘team’-psychologist, dietitian, endocrinologist? That’s a billing code cascade.
But hey, if it works, it works. Just don’t call it ‘medicine.’ Call it capitalism with a scalpel.
See Lo
December 5, 2025 AT 13:2642% remission at 1 year? That’s a 58% failure rate. And you call this ‘effective’? The death rate may be lower than gallbladder surgery-but gallbladder surgery doesn’t require you to take 12 pills a day for the rest of your life.
Also, the ‘95% remission’ with duodenal switch? That’s from a 2007 study with 32 patients. That’s not science. That’s a marketing pamphlet.
And why no mention of the 2023 Lancet paper showing metabolic surgery increases risk of alcohol use disorder by 200%? Oh right-because it’s inconvenient.
Stop selling hope. Start selling data.
:|
Chris Long
December 6, 2025 AT 09:37They’re calling this ‘metabolic surgery’ now? That’s just a fancy name for ‘gut mutilation.’
Back in the day, we ate real food, worked with our hands, and didn’t need some surgeon to cut us open to fix what a bag of chips and a soda caused.
This is what happens when you let weak-minded people outsource their discipline. You don’t fix diabetes with a stapler. You fix it with willpower. And discipline. And maybe not eating the damn donut.
Liv Loverso
December 6, 2025 AT 12:01What if the real problem isn’t the stomach? What if it’s the soul? We’ve turned healing into a technical problem-fix the gut, fix the sugar, fix the life.
But what if diabetes is a symptom of disconnection? From food. From community. From meaning?
Maybe the surgery works because it forces you to slow down. To sit with hunger. To ask: why did I eat that?
It’s not the bypass that cures. It’s the silence after.
Steve Davis
December 6, 2025 AT 20:21I had the bypass in 2020. Lost 110 lbs. Off insulin in 3 weeks. Best thing I ever did.
But you know what? My mom still won’t talk to me. Says I ‘gave up on myself’ by choosing surgery. That I ‘betrayed the natural way.’
She’s 72 and on 6 diabetes meds. I’ve been off all of them for 4 years.
She calls me ‘a science experiment.’
So yeah. It works.
But sometimes, the hardest part isn’t the surgery. It’s the people who love you… but don’t believe you’re worth saving.
Attila Abraham
December 8, 2025 AT 05:10Michelle Machisa
December 9, 2025 AT 19:03I’m a nurse in a bariatric clinic. I’ve seen this play out hundreds of times.
It’s not perfect. But for the person who’s spent 10 years chasing their own tail with diets and pills? This is their lifeline.
Don’t judge the surgery. Judge the system that made them wait this long.
And if you’re considering it? Find a center that does mental health screening. That’s the secret sauce.
Ronald Thibodeau
December 10, 2025 AT 21:55Okay but like… why are we even talking about this like it’s new? I’ve known people who got this done in 2012. It’s not rocket science. Also, the ‘95% remission’ with duodenal switch? That’s for people who weigh 400+ lbs. My cousin’s BMI was 31 and she got the sleeve-she’s still on metformin.
So yeah. Works for some. Not a magic bullet.
Also, why is everyone acting like this is a revelation? We’ve known this since 2007.
Shawn Jason
December 12, 2025 AT 17:26I wonder… if we treated insulin resistance as a systemic stress response instead of a metabolic defect, would we approach this differently?
What if the real intervention isn’t surgical-but societal? Less processed food. More community gardens. More sleep. Less chronic anxiety?
Maybe surgery is the last resort… because we’ve failed to create a world where it wouldn’t be necessary.
Monika Wasylewska
December 14, 2025 AT 14:04Jackie Burton
December 15, 2025 AT 01:46Here’s the real data they won’t show you: 78% of patients who undergo metabolic surgery develop non-alcoholic fatty liver disease within 3 years due to malabsorption-induced lipid dysregulation.
Also, the ‘GLP-1 surge’? That’s just a temporary spike. The gut adapts. The pancreas gets exhausted. Remission isn’t remission-it’s delayed failure.
And the supplements? They’re not just vitamins. They’re synthetic compounds your body can’t properly metabolize.
They’re selling you a slow, silent decline disguised as health.