Every year, millions of Americans skip doses, stop taking meds early, or switch to cheaper alternatives because they can’t afford their prescriptions. Many don’t realize there’s a professional who can help them keep their treatment on track without sacrificing effectiveness-or breaking the bank. That person is the pharmacist.
Medication Therapy Management (MTM) isn’t just another pharmacy service. It’s a structured, patient-centered approach where pharmacists take a deep dive into everything a person is taking-prescriptions, over-the-counter drugs, supplements-and figure out how to make it safer, simpler, and more affordable. And when it comes to generic drugs, pharmacists are the unsung heroes making sure cost-cutting doesn’t mean treatment-cutting.
What Exactly Is Medication Therapy Management?
MTM is a formal service defined by the American Pharmacists Association as a way to optimize how medications work for each individual. It’s not about handing out pills. It’s about asking: Is this drug right for you? Is it working? Are you taking it correctly? And most importantly-can you afford it?
Pharmacists conducting MTM sessions spend 20 to 40 minutes per patient, reviewing every medication on the list. They don’t just look at what’s prescribed-they check for duplicates, interactions, side effects, and whether cheaper alternatives exist. This is where generic drugs come in.
The FDA says generic drugs are just as safe and effective as brand-name versions. They contain the same active ingredients, work the same way, and meet the same strict standards. But they cost 80 to 85% less. That’s not a small difference-it’s life-changing for someone on a fixed income.
Why Pharmacists Are the Key to Generic Drug Success
Most people think switching to a generic is simple: just swap the name on the bottle. But it’s not that easy.
Some drugs have narrow therapeutic indexes-tiny differences in dosage can cause big problems. Think blood thinners like warfarin or seizure meds like phenytoin. Pharmacists know which generics are truly equivalent and which ones might need extra monitoring. They check the FDA’s Orange Book, which rates drug equivalence, and make sure the substitution won’t risk the patient’s health.
But even when generics are perfectly safe, patients still resist. Many believe generics are “weaker” or “inferior.” A study found that 26% of non-adherence is directly tied to cost concerns-and many of those patients are avoiding meds because they don’t trust the cheaper version.
That’s where pharmacists step in. During an MTM session, they don’t just suggest a switch-they explain why it’s safe. They show patients the science. They share stories: “Your neighbor took this same generic for her high blood pressure and saved $300 a month. Her numbers are better now.”
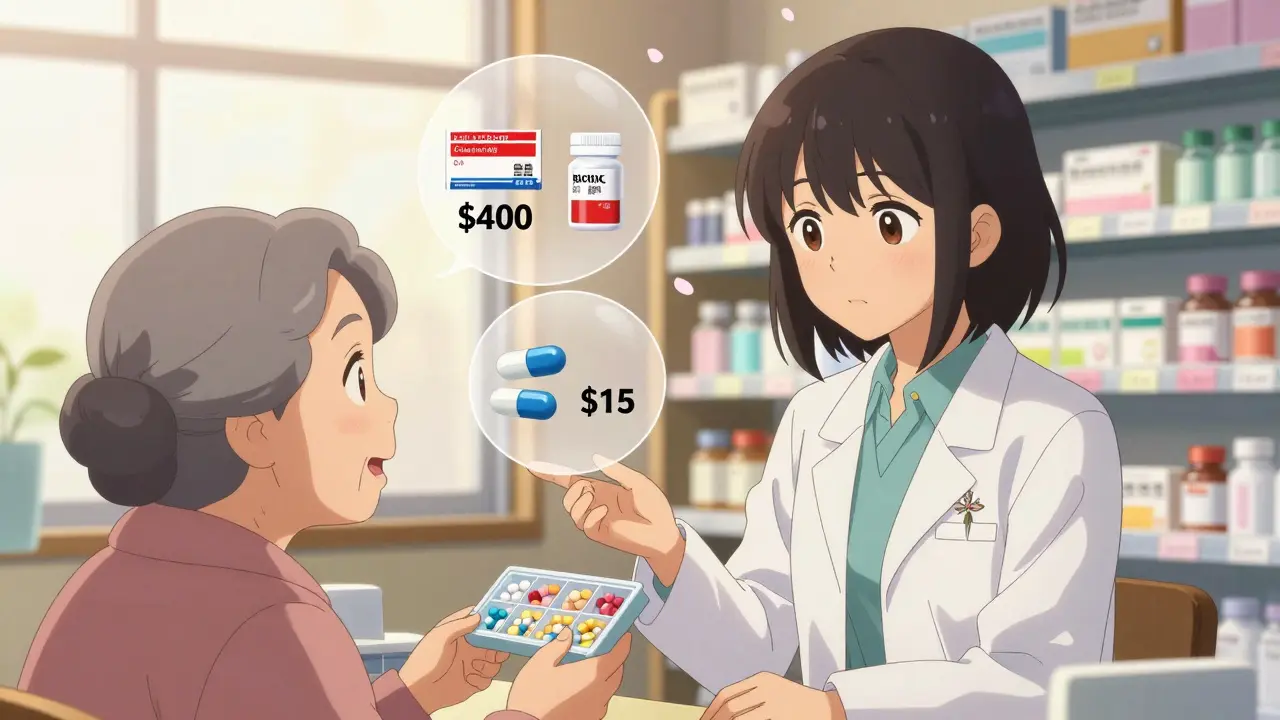
One HealthPartners patient said her MTM pharmacist helped her switch from a $400/month brand-name inhaler to a $15 generic with the same active ingredient. “It literally saved me from choosing between meds and groceries,” she said.
How MTM Differs from Regular Pharmacy Service
At your local pharmacy, the average interaction lasts about 1.7 minutes. It’s a transaction: pay, pick up, go.
MTM is different. It’s a conversation. Pharmacists ask questions like:
- Are you having side effects you haven’t told your doctor about?
- Do you take all your meds at the same time every day?
- Do you know why you’re taking this one?
- Have you ever skipped a dose because it was too expensive?
Studies show MTM sessions uncover an average of 4.2 medication-related problems per patient. That’s more than double what a doctor might catch in a 10-minute visit. And 37% of the cost savings from MTM come specifically from optimizing generic drug use.
Pharmacists don’t just recommend generics-they track outcomes. If a patient switches to a generic and their blood pressure drops too low, the pharmacist follows up. If the new pill causes nausea, they suggest a different generic brand or adjust the timing. They’re not just dispensing-they’re managing.

The Real Impact: Numbers That Matter
The data doesn’t lie. When pharmacists lead MTM programs, results improve across the board:
- Medication adherence increases by an average of 18.7 percentage points.
- Hospital readmissions drop by 23% within 30 days.
- Patients save an average of $214 per month through generic substitutions.
- For every $1 spent on MTM, healthcare systems save $3.17.
One 2022 review of 47 studies found MTM services reduced total annual healthcare costs by $1,247 per patient. And when pharmacists focused on generic drug optimization, those savings jumped even higher.
These aren’t hypotheticals. They’re real outcomes from real patients. A Medicare beneficiary in Ohio cut her monthly drug bill from $512 to $198 after her pharmacist identified three brand-name drugs with equally effective generics. She didn’t change her condition. She didn’t change her treatment. She just got the same results for less.
Challenges Standing in the Way
Despite the proven benefits, MTM still isn’t reaching everyone.
Only 15 to 25% of eligible Medicare beneficiaries actually use the service. Why? Many don’t know it exists. Others are told by their pharmacy, “We don’t offer it”-because reimbursement is too low.
Medicare pays $50 to $150 per Comprehensive Medication Review. But private insurers? Often just $25 to $75. For a 30-minute session that requires documentation, follow-up, and coordination with doctors, that’s not enough to cover time and overhead.
Another hurdle? Technology. Only 38% of community pharmacies have seamless electronic health record integration. That means pharmacists are still printing, faxing, or manually entering notes-slowing things down and increasing errors.
And state laws vary. Only 42 states give pharmacists explicit authority to make changes to prescriptions under collaborative practice agreements. In the rest, they can recommend-but not act-without a doctor’s approval.
What Pharmacists Need to Do It Right
Doing MTM well isn’t something you learn on the job. It takes training.
Pharmacists need to understand:
- Therapeutic equivalence-how to read the FDA’s Orange Book ratings (A = equivalent, B = not equivalent)
- Pharmacoeconomics-how to balance cost and clinical outcomes
- Communication skills-how to explain generics without sounding dismissive
- Documentation-using SOAP notes (Subjective, Objective, Assessment, Plan) to track every change
Certifications like BCPS (Board Certified Pharmacotherapy Specialist) or BCACP (Board Certified Ambulatory Care Pharmacist) help. But even without them, structured training programs-usually 40 to 60 hours-can prepare pharmacists to lead MTM sessions effectively.
Successful programs use standardized tools like the Medication Appropriateness Index (MAI), which scores each drug on 10 criteria: Is it needed? Is it effective? Is the dose right? Is it affordable?
Where MTM Is Headed
MTM is growing. In 2022, 12.7 million Medicare beneficiaries received MTM services. Commercial plans cover another 85 million Americans.
Telehealth has made it easier. Since the pandemic, 63% of MTM programs now include virtual visits. Patients can talk to their pharmacist from home-no travel, no waiting.
And new tech is emerging. Some pharmacists now use pharmacogenomics-testing how a person’s genes affect drug metabolism-to decide whether a brand-name or generic version is better suited for them. For example, someone who metabolizes a drug too slowly might need a different generic than someone who clears it quickly.
The American Pharmacists Association is pushing for standardized reporting on generic drug savings by 2024. That means pharmacies will soon be able to show exactly how much money they’ve saved patients-not just guess.
By 2025, 78% of health systems plan to expand pharmacist roles in MTM. The Bureau of Labor Statistics predicts 4.6% growth in pharmacist jobs through 2032-mostly because of these clinical roles.
What You Can Do
If you’re on Medicare Part D, you’re eligible for MTM. Call your pharmacy and ask: “Do you offer Medication Therapy Management?” If they say no, ask why. If it’s because of reimbursement, ask them to connect you with a local clinic or telehealth provider that does.
If you’re on a private plan, check your benefits. Many employers offer MTM as part of wellness programs. You might not even know it’s available.
And if you’re taking generics and still worried they’re not working? Talk to your pharmacist. They’re trained to answer those questions. They’ve seen it before. They can show you the evidence. And they might just save you hundreds a month.
Medication therapy management isn’t about replacing doctors. It’s about giving patients a true partner-one who knows drugs inside and out, who cares about cost as much as care, and who won’t let financial barriers get in the way of health.
What is Medication Therapy Management (MTM)?
Medication Therapy Management (MTM) is a service provided by pharmacists to help patients use their medications safely and effectively. It includes reviewing all prescriptions, over-the-counter drugs, and supplements to identify problems like interactions, unnecessary meds, or cost issues. The goal is to improve health outcomes and reduce side effects or hospital visits.
Can pharmacists really switch my brand-name drugs to generics?
Pharmacists can recommend generic substitutions, but whether they can make the switch depends on your state’s laws and your prescriber’s rules. In most cases, they can suggest the change and communicate with your doctor. In 42 states, they can make the switch directly under a collaborative practice agreement. Even if they can’t change it themselves, they’ll help you get approval.
Are generic drugs really as good as brand-name ones?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict manufacturing standards. The only differences are in inactive ingredients (like fillers) and packaging. For 90% of drugs, generics work identically. Pharmacists use the FDA’s Orange Book to confirm equivalence before recommending a switch.
Who qualifies for MTM services?
Medicare Part D beneficiaries who take multiple chronic condition medications, have high drug costs, or are at risk for hospitalization typically qualify. Commercial insurers also offer MTM to members with complex medication regimens. You don’t need to ask for it-your plan should notify you if you’re eligible. But if you’re unsure, call your pharmacy or insurer to ask.
How much does MTM cost?
MTM services are free for Medicare Part D beneficiaries. For commercial insurance, it’s usually covered as part of your plan benefits. There’s no out-of-pocket cost for the consultation. The pharmacy or insurer handles the billing. You only pay for your medications-same as always.
How long does an MTM session take?
The first session usually takes 20 to 40 minutes. Follow-up visits are shorter-10 to 20 minutes. You’ll meet one-on-one with a pharmacist, either in person or over the phone. They’ll review your full medication list, ask about side effects, and create a personalized action plan. You’ll get a written summary and a list of next steps.

LALITA KUDIYA
January 6, 2026 AT 14:55Poppy Newman
January 8, 2026 AT 09:35Anthony Capunong
January 10, 2026 AT 02:52Jessie Ann Lambrecht
January 11, 2026 AT 04:49Emma Addison Thomas
January 11, 2026 AT 13:52Mina Murray
January 11, 2026 AT 23:44Rachel Steward
January 12, 2026 AT 10:12Christine Joy Chicano
January 13, 2026 AT 04:20Adam Gainski
January 13, 2026 AT 15:06Anastasia Novak
January 15, 2026 AT 03:02Jonathan Larson
January 15, 2026 AT 21:16Elen Pihlap
January 17, 2026 AT 01:22Sai Ganesh
January 17, 2026 AT 02:15Paul Mason
January 17, 2026 AT 04:46Katrina Morris
January 18, 2026 AT 22:27