Enlarged Prostate Symptom Tracker
Rate how often you experience each symptom over the past week (0 = Never, 1 = Rarely, 2 = Sometimes, 3 = Often, 4 = Very Often)
Overall Symptom Severity:
Symptom Breakdown:
Dealing with an enlarged prostate can feel like an endless round of bathroom trips, waking up at night, and wondering if there’s anything you can actually do about it. This guide walks you through what’s happening inside the body, which everyday habits can keep symptoms in check, and which medical options are worth a closer look.
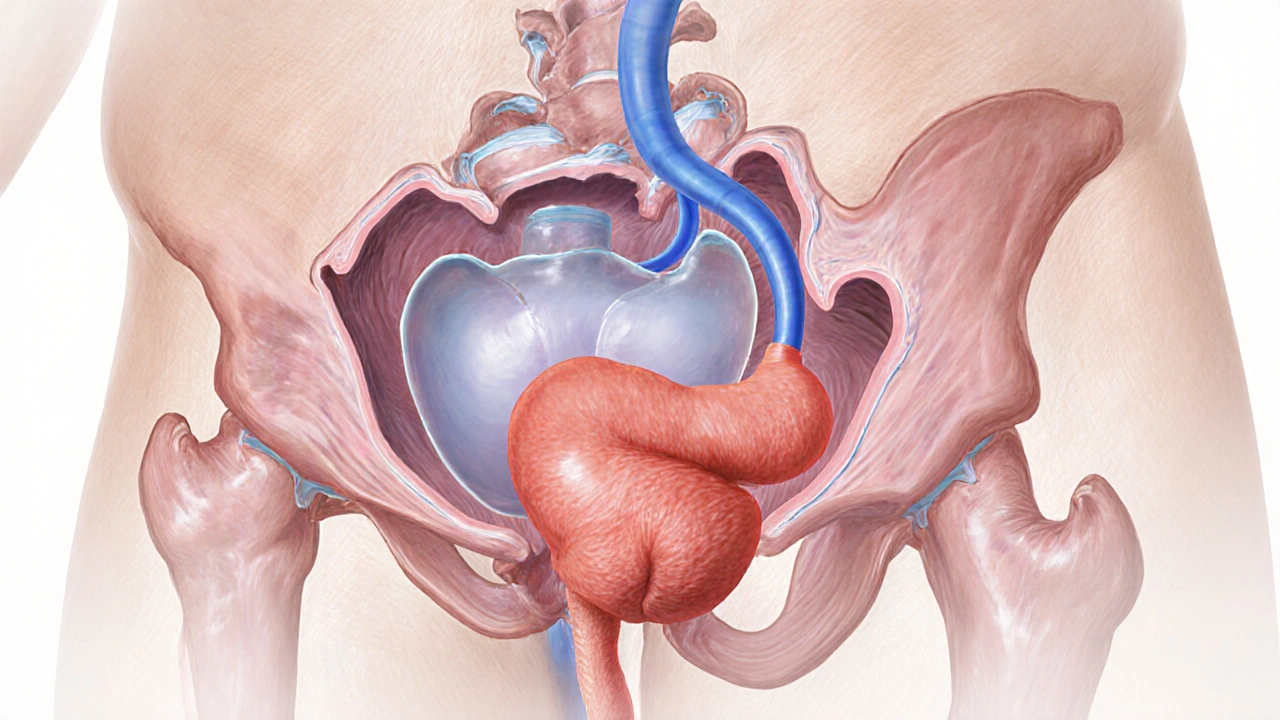
What an Enlarged Prostate Actually Is
When most men hear the term "enlarged prostate," they picture a painful swelling. In reality, the condition-clinically called Benign Prostatic Hyperplasia (BPH)-is a non‑cancerous growth of the gland that sits beneath the bladder. As the prostate grows, it squeezes the urethra, making it harder for urine to flow out.
Key facts:
- About 50% of men over 50 experience some degree of BPH.
- The prostate can double in size, reaching 30-40cc in severe cases.
- Most men never need surgery; lifestyle tweaks and medication manage the majority of symptoms.
Typical Symptoms and How to Spot Them
Symptoms fall into two groups: storage (how the bladder holds urine) and voiding (how it empties). Common signs include:
- Frequent urination, especially at night (nocturia).
- Urgent need to go, sometimes with a weak stream.
- Feeling that the bladder isn’t empty after peeing.
- Dribbling at the end of a void.
If any of these start to affect daily life, it’s time to take action.
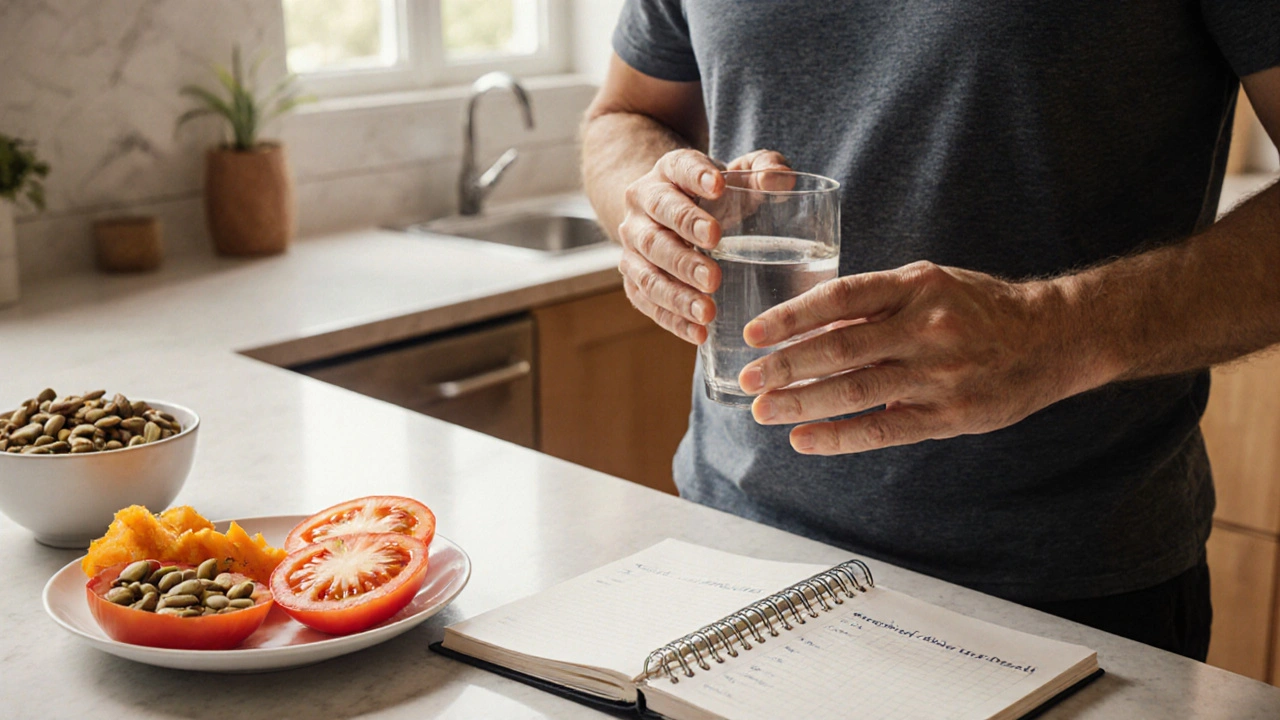
Lifestyle Changes That Actually Help
Small daily habits can reduce pressure on the bladder and improve flow. Here’s a checklist you can start tomorrow:
- Fluid timing: Limit drinks two hours before bedtime to cut nocturia.
- Limit irritants: Cut back on caffeine, alcohol, and spicy foods, which can inflame the bladder.
- Stay active: Regular walking or low‑impact exercise improves pelvic circulation.
- Pelvic floor training: Perform pelvic floor exercises (often called Kegels) 10seconds on, 10seconds off, 5-10 repetitions, three times a day. Studies show a 20% improvement in urinary flow after six weeks.
- Balanced diet: Emphasize fruits, vegetables, and whole grains. A diet rich in lycopene (tomatoes) and zinc (pumpkin seeds) correlates with modest reductions in prostate volume.
When Over‑the‑Counter Isn’t Enough: Medical Options
If symptoms linger after lifestyle tweaks, talking to a urologist opens the door to proven medications. The two main classes are:
| Class | Common Drugs | How They Work | Typical Benefits | Side‑effects |
|---|---|---|---|---|
| Alpha‑blockers | Tamsulosin, Alfuzosin | Relax smooth muscle in the prostate and bladder neck | Quick relief (within days), improved flow | Dizziness, low blood pressure |
| 5‑alpha‑reductase inhibitors | Finasteride, Dutasteride | Block conversion of testosterone to DHT, shrinking prostate size | Long‑term reduction in prostate volume, lower risk of surgery | Reduced libido, erectile dysfunction (usually resolves) |
Most doctors start patients on an alpha‑blocker for fast symptom relief, then add a 5‑alpha‑reductase inhibitor if the prostate is significantly enlarged (over 30cc).
Herbal and Complementary Approaches
Some men explore natural supplements. The most studied is saw palmetto. Clinical trials show modest symptom improvement in about 30% of users, but results are inconsistent. If you try it, keep the dose at 320mg daily and discuss it with your doctor to avoid interactions.
Other options that have limited evidence include:
- Beta‑sitosterol (plant sterol) - may improve flow speed.
- Pygeum africanum - some Asian studies suggest reduced nighttime urination.
Remember: “natural” doesn’t mean “risk‑free.” Always verify purity and stay within recommended dosages.
Monitoring Progress: Tests and Red‑Flags
Regular check‑ups help you and your clinician gauge if the plan works.
- PSA test (Prostate‑Specific Antigen) - while mainly a cancer screen, rising PSA can indicate prostate growth.
- Ultrasound measurement - gives an exact prostate volume (in cubic centimeters).
- Urinary flow study - measures peak flow rate; values below 15mL/s often trigger medication escalation.
Seek urgent care if you notice:
- Sudden inability to urinate (acute urinary retention).
- Blood in urine or semen.
- Severe pain in the lower abdomen.
Putting It All Together: A Personal Action Plan
Here’s a simple 4‑week roadmap you can follow:
- Week1: Log bathroom trips, note triggers, and start fluid timing.
- Week2: Add pelvic floor exercises and a 20‑minute walk most days.
- Week3: Schedule an appointment with a urologist; bring your symptom log.
- Week4: If medication is prescribed, begin the regimen and track side‑effects.
Re‑evaluate every month. Most men see noticeable relief within three months of combining lifestyle changes with medication.
Frequently Asked Questions
Can diet alone shrink an enlarged prostate?
Diet helps manage symptoms but rarely shrinks the gland dramatically. Foods rich in lycopene and zinc can modestly slow growth, while excessive red meat and dairy may aggravate symptoms.
Are alpha‑blockers safe for older men with low blood pressure?
Alpha‑blockers can lower blood pressure, so doctors usually start with a low dose and monitor standing systolic pressure. If dizziness occurs, dosage adjustment or an alternative medication may be needed.
How long before 5‑alpha‑reductase inhibitors show results?
These drugs work by shrinking the prostate, so noticeable improvement typically appears after 3-6months of consistent use.
Is nocturia always a sign of BPH?
Not always. Heart failure, sleep apnea, and high fluid intake can also cause nighttime trips. A thorough evaluation helps pinpoint the true cause.
When should I consider surgery?
Surgery is usually reserved for severe obstruction, recurrent urinary retention, bladder stones, or when medication fails after 6-12months. Procedures range from minimally invasive laser therapy to traditional TURP.

Mansi Mehra
October 10, 2025 AT 17:41The guide provides a thorough overview of BPH symptom management. It could benefit from clearer headings.
Danielle Spence
October 10, 2025 AT 17:48It is disheartening to see health content that downplays lifestyle changes. People should prioritize proven interventions over quick fixes.
Dhanu Sharma
October 10, 2025 AT 17:54Nice tool but the UI feels a bit clunky.
Edward Webb
October 10, 2025 AT 18:01Understanding the psychological impact of urinary symptoms is as crucial as addressing the physical aspects. The guide could incorporate coping strategies for anxiety related to frequent night-time trips.
Snehal Suhane
October 10, 2025 AT 18:07Oh great, another "complete" guide that pretends to know everything while ignoring the nuance of individualized care. Guess we’re all supposed to trust a one‑size‑fits‑all calculator.
Ernie Rogers
October 10, 2025 AT 18:13Seems decent but could use more American clinical guidelines.
Eunice Suess
October 10, 2025 AT 18:19This tracker is kinda helpful, but the wording is all over the place. It needs a proper edit.
Anoop Choradia
October 10, 2025 AT 18:26The purported objectivity of this symptom tracker is questionable, given the undisclosed affiliations with pharmaceutical interests that may bias the recommendations presented herein.
bhavani pitta
October 10, 2025 AT 18:32While the interface appears polished, I find the emphasis on quantifying discomfort rather than addressing underlying etiologies to be profoundly misguided.
Brenda Taylor
October 10, 2025 AT 18:39Honestly this thing feels like a gimmick 😒
virginia sancho
October 10, 2025 AT 18:45Even if the guide isn’t perfect, it can still serve as a starting point for men to track symptoms and discuss them with doctors.
Namit Kumar
October 10, 2025 AT 18:51Looks like a typical pharma‑sponsored tool 😏
Sam Rail
October 10, 2025 AT 18:57Sure, but sometimes simple advice is what folks need.
Taryn Thompson
October 10, 2025 AT 19:04Excellent point. Incorporating mindfulness exercises could alleviate the anxiety you mentioned.
Lisa Lower
October 10, 2025 AT 19:11First of all, kudos for putting together something that actually attempts to quantify a condition that many men suffer in silence.
Secondly, the layout is surprisingly intuitive, allowing users to input data without feeling overwhelmed.
Third, the color‑coded severity bar provides instant visual feedback, which can be motivating for those tracking progress over time.
Fourth, the inclusion of both daytime and nighttime frequency acknowledges the full spectrum of BPH symptoms.
Fifth, the weak stream and difficulty starting metrics address concerns that are often under‑discussed in mainstream articles.
Sixth, the “feeling of incomplete emptying” item captures a nuance that many clinicians overlook.
Seventh, by aggregating these scores into an overall percentage, the tool offers a clear, digestible summary.
Eighth, the accompanying recommendations, though brief, give users a tangible next step rather than leaving them in a vacuum.
Ninth, the design is responsive, meaning it works well on both desktop and mobile devices, increasing accessibility.
Tenth, the code snippets are neatly organized, suggesting that future updates could be rolled out smoothly.
Eleventh, the progress bar animation adds a subtle touch of polish without being distracting.
Twelfth, the open‑source nature of the script invites community contributions, which can only improve its accuracy over time.
Thirteenth, the tool encourages men to talk to their physicians armed with concrete data, potentially leading to better-informed treatment decisions.
Fourteenth, the language used is straightforward, avoiding medical jargon that could alienate lay readers.
Fifteenth, the overall approach of empowering patients through self‑monitoring aligns with modern, patient‑centered care models.
Finally, while no tool can replace professional medical advice, this tracker serves as a valuable bridge between personal experience and clinical consultation.
Dana Sellers
October 10, 2025 AT 19:16If you’re not following the guide, you’re basically ignoring your health.
Damon Farnham
October 10, 2025 AT 19:23Indeed, neglecting such advice, especially when it’s freely available, reflects a troubling disregard for personal responsibility, and it’s disconcerting, to say the least.
Gary Tynes
October 10, 2025 AT 19:29Hey, maybe try adding a section on diet changes-it could help more than just tracking.
Marsha Saminathan
October 10, 2025 AT 19:35Wow this guide really sparks a fire of curiosity; the interactive elements are vibrant and the advice feels fresh and relatable.
Justin Park
October 10, 2025 AT 19:42One wonders whether quantifying symptoms truly captures the lived experience 🤔