Drug Interaction Checker
Check Your Medications
Interaction Results
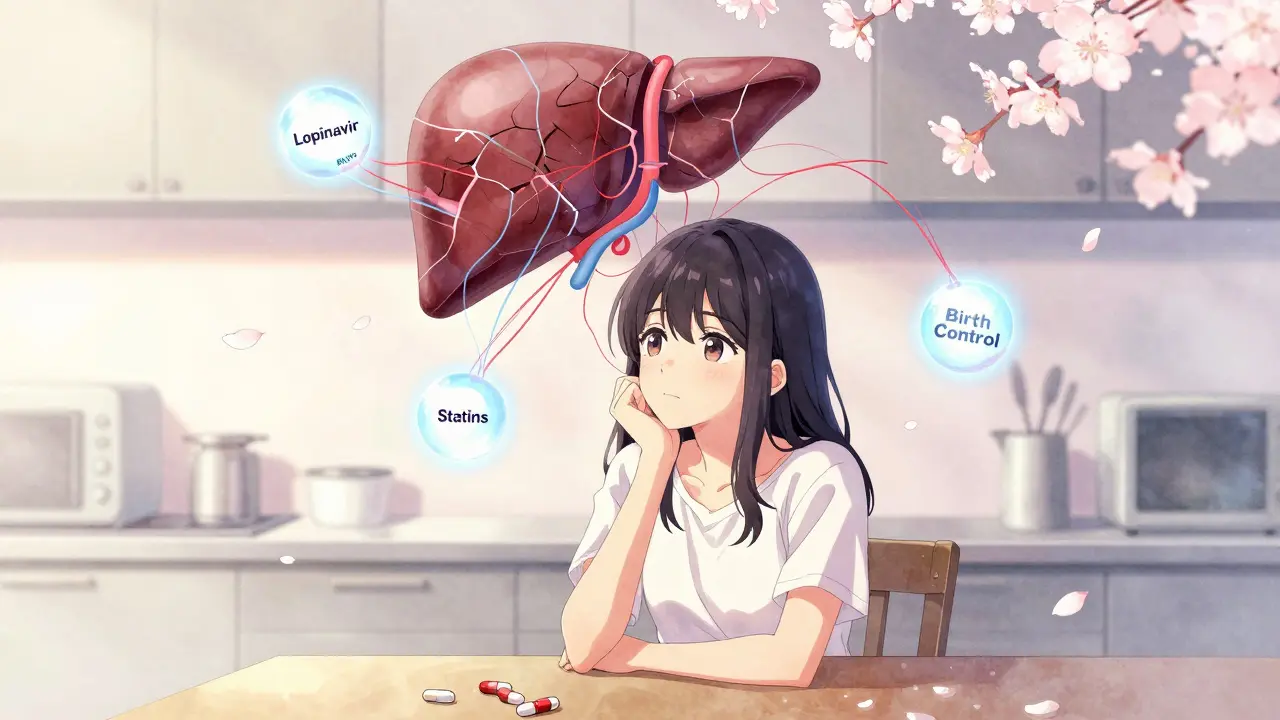
The real problem with lopinavir/ritonavir isn’t that it doesn’t work - it’s that it changes everything else in your body’s drug metabolism. This combo, once a backbone of HIV treatment, isn’t just another pill. It’s a chemical wrench thrown into the finely tuned machinery of your liver enzymes. And if you’re taking anything else - even something as simple as a statin or a birth control pill - you might not realize how much it’s messing with your system.
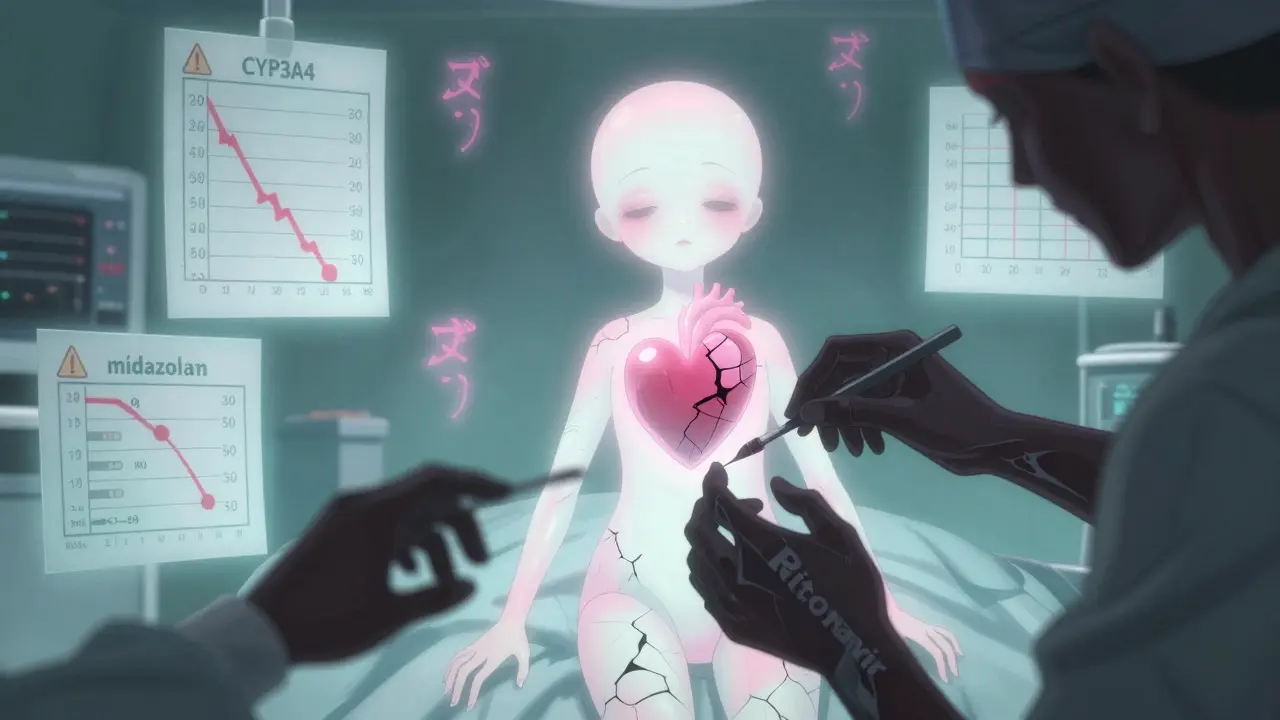
At its core, lopinavir/ritonavir (sold as Kaletra) works because of one trick: ritonavir, given in a tiny 100mg dose, doesn’t treat HIV at all. Instead, it shuts down a key enzyme called CYP3A4. This enzyme normally breaks down lopinavir, so without ritonavir, lopinavir would vanish from your bloodstream in under 7 hours. With ritonavir blocking CYP3A4, lopinavir sticks around long enough to work - twice a day instead of three. Simple, right? Not even close.
How Ritonavir Actually Works - And Why It’s So Dangerous
Ritonavir doesn’t just block CYP3A4 like a simple key in a lock. It destroys it. In lab studies, ritonavir binds to the enzyme so tightly that it permanently damages it. It doesn’t just sit there - it tears apart the enzyme’s structure, breaks its heme group, and even glues itself to the protein. This isn’t temporary inhibition. It’s chemical sabotage. And that’s why its effects last for days, even after you stop taking it.
But here’s the twist: ritonavir doesn’t just inhibit. It also induces other enzymes - CYP1A2, CYP2B6, CYP2C9, CYP2C19. That means it can speed up the breakdown of some drugs while slowing down others. It’s like a switch that turns some processes off and others on. No other boosting agent does this. Cobicistat? Clean. Selective. Ritonavir? A sledgehammer.
For example, if you’re on warfarin (a blood thinner), ritonavir can make it less effective by speeding up its breakdown through CYP2C9. That means your INR drops. You’re at risk of clots. But if you’re on midazolam (a sedative), ritonavir can make its levels spike by 500%. That’s not just drowsiness - that’s respiratory arrest waiting to happen. Anesthesiologists have documented cases where patients on lopinavir/ritonavir needed 80% less fentanyl or midazolam during surgery. One wrong dose, and you don’t wake up.
The Interaction List Is Longer Than Your Phone Contacts
The Liverpool HIV Interactions Database, updated in July 2023, lists 1,247 potential drug interactions with lopinavir/ritonavir. That’s more than double the number for newer combos like darunavir/cobicistat. Let’s break down some of the most dangerous ones:
- Tacrolimus (transplant drug): Levels spike 300-500%. Without a 75% dose reduction, you risk kidney failure.
- Rivaroxaban (blood thinner): Contraindicated. The combo can cause life-threatening bleeding.
- Methadone: Ritonavir speeds up its metabolism. Doses often need to be increased by 20-33% to avoid withdrawal - but too much and you overdose.
- Statins (like simvastatin, atorvastatin): Risk of rhabdomyolysis (muscle breakdown) increases dramatically. Fluvastatin or pravastatin are safer.
- Hormonal contraceptives: Ritonavir cuts estrogen levels by over 50%. Birth control pills become unreliable. Backup methods aren’t optional.
- Voriconazole (antifungal): Unpredictable levels. Sometimes too low (treatment fails), sometimes too high (liver toxicity). Contraindicated.
And these are just the common ones. There are dozens more - from antidepressants to anti-seizure meds to cancer drugs. Every single one needs to be checked before you even think about starting lopinavir/ritonavir.
Why It’s Still Used - And Where It Hangs On
You’d think a drug with this many risks would vanish. But it hasn’t. In low- and middle-income countries, lopinavir/ritonavir still makes up 28% of first-line HIV regimens. Why? Price. In PEPFAR programs, it costs $68 per person per year. Newer drugs like dolutegravir cost $287. When you’re treating millions with limited budgets, cost wins.
But even there, it’s fading. UNAIDS projects its use will drop to 12% by 2027. Why? Because patients can’t tolerate it. A 2022 meta-analysis found lopinavir/ritonavir regimens had 37% higher discontinuation rates than integrase inhibitors - mostly due to nausea, diarrhea, and liver damage. In high-income countries, it’s basically extinct. The U.S. DHHS stopped recommending it in 2015. The WHO still lists it as essential, but only as a fallback.
The Hidden Risk: What Happens When You Stop
Here’s something no one talks about: even after you stop lopinavir/ritonavir, the enzyme damage doesn’t reset overnight. CYP3A4 regeneration takes days. That means if you switch to another drug - say, a new antiviral or a painkiller - your body still thinks ritonavir is there. You might take a normal dose of a drug that’s now being broken down too slowly. You overdose. Slowly.
This is why the 2023 “Paxlovid rebound” phenomenon is so telling. Paxlovid uses the same ritonavir boosting trick. Patients would finish the 5-day course, feel better, then get sick again. Why? Because ritonavir’s half-life (3-5 hours) is shorter than nirmatrelvir’s (6-10 hours). Once ritonavir clears, CYP3A4 starts coming back - but too slowly. Nirmatrelvir levels crash. The virus rebounds. It’s a timing nightmare.
Same thing happens with lopinavir. If you stop it and immediately start another drug metabolized by CYP3A4, you’re gambling with your liver, your kidneys, your heart.

What Clinicians Actually Do - And How You Can Protect Yourself
Doctors don’t guess. They use tools. The Liverpool HIV Interactions Database gets 2.8 million hits a year. Pharmacists spend 15-20 minutes per patient just checking interactions. That’s not a suggestion - it’s standard care. If your provider skips this step, walk out.
Here’s what you need to do:
- Give your doctor a complete list of every medication, supplement, and OTC drug you take - including vitamins, herbal teas, and recreational substances.
- Ask: “Is lopinavir/ritonavir safe with everything I’m on?” Don’t accept a yes without proof.
- Get your liver enzymes checked before starting and every 4-6 weeks after.
- If you’re on hormonal birth control, use condoms or an IUD. Period.
- If you’re scheduled for surgery, tell your anesthesiologist at least a week in advance. They need to adjust sedatives.
- Never switch drugs without a pharmacist review. Even switching from one statin to another can be deadly.
And if you’re in a resource-limited setting? Advocate. Push for alternatives. Dolutegravir isn’t just safer - it’s simpler. One pill, once a day. No interactions. No monitoring. No guesswork.
The Future: A Dying Tool With a Legacy
Lopinavir/ritonavir was revolutionary in 2000. It turned a once-daily, toxic, unreliable regimen into a twice-daily, life-saving one. But science moved on. Newer drugs don’t need chemical sledgehammers to work. They’re designed to be clean. Predictable. Safe.
Today, its only real role is as a bridge - in places where better options don’t exist. Even then, it’s a bridge with holes. Every time it’s prescribed, it’s a risk assessment. Every interaction is a potential emergency. Every patient needs to be treated like a minefield.
It’s not the drug that’s broken. It’s the system that still uses it. We’ve known for years that integrase inhibitors are better. We’ve known for years that ritonavir’s interaction profile is a nightmare. The question isn’t whether we should stop using it. The question is: why are we still letting people take it without knowing exactly what they’re signing up for?

Alex Ogle
February 9, 2026 AT 13:34So let me get this straight - ritonavir doesn’t just inhibit CYP3A4. It *murders* it. Like, full-on, forensic-level destruction. Heme group? Gone. Protein structure? Glued shut. It’s not a pharmacokinetic tweak - it’s a biochemical crime scene.
And the worst part? You think you’re done with it after you stop taking it. Nope. Your liver’s still reeling. Days later, you take a normal dose of something - say, a painkiller - and boom. You’re in the ER because your body’s still operating under the assumption that the enzyme’s dead.
This isn’t a drug interaction. It’s a chemical hostage situation. And we’re still prescribing it like it’s just another pill. I’m not even mad. I’m just... disappointed.
Tatiana Barbosa
February 10, 2026 AT 09:16Y’all need to stop treating this like a textbook problem. This is real life. I’ve seen patients on ritonavir who thought their birth control was fine - until they got pregnant. Again. And again. No one told them estrogen gets shredded by CYP3A4 suppression. No one.
It’s not about the science. It’s about the silence. Doctors skip the interaction check because it’s ‘too time-consuming.’ Pharmacists are overworked. Patients are scared to ask. And the system just keeps rolling. We need mandatory pharmacist reviews before every prescription. Period. No exceptions.
Simon Critchley
February 10, 2026 AT 10:14LOL. ‘Chemical sabotage’? Nah. It’s just enzyme kinetics on steroids. Ritonavir’s a suicide inhibitor - covalent binding, irreversible inactivation. Classic. Cobicistat? Pfft. That’s just a polite version of the same thing - no heme destruction, no induction, no drama. But let’s be real: the real issue isn’t ritonavir. It’s that we’re still using a 2001-era backbone in 2024.
Also, ‘Paxlovid rebound’? That’s not a rebound. That’s a pharmacokinetic echo. CYP3A4 regen lag. Same mechanism. Same problem. We knew this in 2017. Why are we still pretending it’s new?
Karianne Jackson
February 11, 2026 AT 01:09I took this for 6 months. I lost 15 pounds. Couldn’t sleep. Felt like my liver was screaming. Then I stopped. And guess what? My anxiety got worse. I thought it was ‘mental.’ Turns out it was the drug leaving my system. No one warned me. No one. This isn’t medicine. It’s a gamble.
Andy Cortez
February 11, 2026 AT 13:32lol so you're telling me the 'miracle drug' that saved hiv patients is actually a poison that ruins your liver and makes birth control useless? wow. i'm shocked. totally didn't see that coming. also, why is this still a thing? because big pharma? because the government? because we're all just too lazy to read the 1247 interactions list? lol. i'm out.
Jessica Klaar
February 13, 2026 AT 03:01I work in a clinic in rural Texas. We still use lopinavir/ritonavir because it’s the only thing we can afford. I wish we had dolutegravir. We really do.
But here’s what I’ve learned: patients who know what they’re up against? They’re careful. They track their meds. They tell us about every herb, every OTC pill, every vape they’re using.
It’s not the drug. It’s the lack of education. We need to stop treating this like a secret. Talk to people. Give them the full picture. They’re smarter than we think.
Patrick Jarillon
February 15, 2026 AT 01:37Let me guess - this is all a distraction. CYP3A4 isn’t the problem. The real issue? The WHO and CDC are pushing this to keep people dependent. Think about it: if you switch to dolutegravir, you need less monitoring. Less blood tests. Less doctor visits. Less data collection. Who benefits? Big Pharma? The government? The surveillance state?
And why is there no public warning about ritonavir’s ‘chemical sabotage’? Because they don’t want you to know how much control they have. You think this is science? It’s control. And you’re the experiment.
John Watts
February 16, 2026 AT 15:11Hey - I’m a nurse in Atlanta. I’ve seen this firsthand. One patient on ritonavir took a normal dose of simvastatin. Got rhabdo. ICU. Two weeks. Lost 40% of his muscle mass.
But here’s the thing - he didn’t even know he was on a high-risk combo. His doctor just said, ‘Here’s your HIV meds.’ No warning. No handout. Nothing.
So I started printing out the Liverpool interaction list. Laminating it. Handing it to every patient. It’s not perfect. But it’s something. If you’re on this combo - get the list. Read it. Bring it to every appointment. You’re your own best advocate.
Randy Harkins
February 17, 2026 AT 05:58Thank you for writing this. 🙏
As someone who’s been on HIV meds for 12 years, I can say this: the shift from lopinavir/ritonavir to integrase inhibitors was the single best thing that happened to my health. No more nausea. No more weird drug interactions. Just… life.
To anyone reading this: if you’re still on this combo - please, please ask your doctor about switching. It’s not about being ‘non-compliant.’ It’s about being smart. You deserve better. 💙
Chima Ifeanyi
February 17, 2026 AT 12:35Let’s cut the euphemisms. Ritonavir isn’t ‘boosting.’ It’s a metabolic terrorist. It doesn’t just interfere - it hijacks. It creates chaos. And the fact that we still use it in LMICs isn’t ‘cost-effective’ - it’s colonial. We’re giving people a drug that requires a PhD-level understanding of pharmacokinetics just to survive.
Meanwhile, dolutegravir costs $287/year. But in the U.S., it’s $15,000. So we ship the cheap, dangerous version to Africa and call it ‘aid.’ That’s not healthcare. That’s exploitation.
Tori Thenazi
February 17, 2026 AT 13:40Okay, but have you considered… what if CYP3A4 isn’t even the real issue? What if it’s the *glyphosate*? Or the *5G*? Or the *fluoride*? I read somewhere that ritonavir’s ‘chemical sabotage’ is actually just a side effect of modern toxins in our water supply. And the pharmaceutical industry is hiding it. They don’t want you to know that your liver is being poisoned by… *corporate greed*.
Also, my cousin’s neighbor’s dog got sick after eating a pill. Coincidence? I think not.
Elan Ricarte
February 17, 2026 AT 17:37They call it ‘boosting.’ I call it chemical rape. You take one pill, and suddenly your body’s metabolism is a warzone. One enzyme dead. Two others turned into overeager interns. Your statin? Gone. Your birth control? Useless. Your surgery sedative? Now a death sentence.
And the worst part? The people who designed this knew. They knew. And they still sold it. Not because it was better. Because it was cheaper. And now, we’re the ones cleaning up the mess. While they cash in on the next ‘breakthrough.’
Lyle Whyatt
February 19, 2026 AT 15:48I’m an Australian pharmacist. We phased out lopinavir/ritonavir in 2019. But I still get calls from patients overseas - mostly from Africa and Southeast Asia - asking if they can switch.
The answer? Yes. But it’s not simple. You need to wait 7–10 days after stopping ritonavir before starting a new drug. Why? Because CYP3A4 doesn’t regenerate overnight. It’s like rebooting a corrupted server - and you can’t just hit ‘restart.’
So if you’re thinking about switching - don’t just swap pills. Talk to a specialist. Get your enzyme levels checked. And if your provider says ‘it’s fine’ - get a second opinion. This isn’t a routine switch. It’s a minefield.
Susan Kwan
February 20, 2026 AT 20:20Wow. So after 20+ years of clinical use, we’re only now realizing that ritonavir is basically a molecular grenade? How many people died before someone said, ‘Maybe we shouldn’t do this?’
And yet - still listed as ‘essential’ by WHO. Because ‘cost-effective.’
Let me guess - next year they’ll add ‘CYP3A4 suppression’ to the list of ‘mild side effects’ alongside ‘dizziness’ and ‘mild nausea.’
At this point, I’m not even surprised.
Tom Forwood
February 21, 2026 AT 05:16Biggest takeaway? If you’re on lopinavir/ritonavir - you’re not just taking a drug. You’re managing a system.
It’s not like taking insulin or metformin. This is like running a nuclear reactor with a single control panel. One wrong move - boom.
So if you’re on this - get a med sync. Talk to your pharmacist. Keep a log. Use a pill organizer. Set phone reminders. And if you’re ever scheduled for surgery - tell them. Twice. Write it down. Send an email. Call the anesthesiologist.
Because if you don’t - no one else will.