Back in 2015, the FDA scrapped the old A, B, C, D, X pregnancy categories that doctors and patients had used for decades. You might still hear them mentioned - but they’re gone. And if you’re trying to figure out whether a medication is safe during pregnancy or while breastfeeding, those letters won’t help you anymore. The new system doesn’t give you a quick grade. It gives you real, detailed information. But only if you know how to read it.
What Replaced the Old Pregnancy Letters?
The old system was simple: A was safest, X was dangerous. But it was misleading. A drug labeled B didn’t mean it was safe - just that animal studies looked okay and human data was thin. C meant risk couldn’t be ruled out - which applied to 70% of all prescription drugs. That didn’t help anyone make a decision. The new system, called the Pregnancy and Lactation Labeling Rule (PLLR), replaced those letters with three clear subsections in every drug’s official labeling: Pregnancy, Lactation, and Females and Males of Reproductive Potential.Reading the Pregnancy Section (8.1)
This part has three key pieces you need to focus on: Risk Summary, Clinical Considerations, and Data.Risk Summary doesn’t say "safe" or "not safe." It tells you the background risk of birth defects - which is about 3% in any pregnancy - and then says whether the drug increases that risk. For example: "Exposure to this drug in the first trimester is associated with a 1.5-fold increased risk of neural tube defects compared to the background rate of 2-4%." That’s useful. It doesn’t scare you. It just gives you context. You’re not just asking "Is this dangerous?" You’re asking, "How much more dangerous is it than what already happens?"
Clinical Considerations is where the action is. This section tells you what to do. Does the drug need dose adjustments during pregnancy? Should you monitor fetal growth every four weeks after 20 weeks? Is there a specific time in pregnancy when the risk is highest? This is the part your doctor should be reading aloud to you.
Data is the fine print. It tells you what studies were done - how many women, how they were followed, what limitations existed. It might say "retrospective cohort of 800 pregnancies" or "no controlled studies in humans." You don’t need to memorize this, but if your doctor says "the data is limited," this is why.
Understanding Lactation Labeling (8.2)
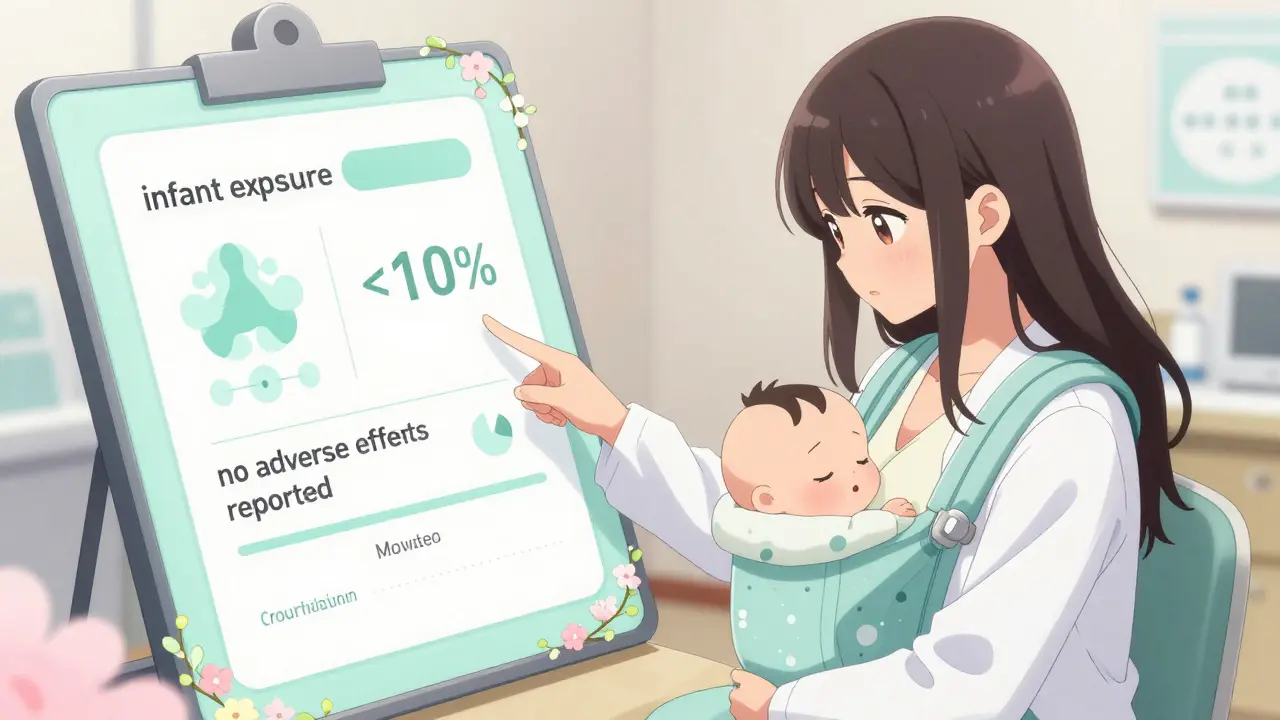
Breastfeeding safety used to be an afterthought. Now it’s required. This section answers three things: How much of the drug gets into breast milk?, What’s the baby’s exposure?, and Are there any reported effects?Look for numbers like "infant exposure is less than 10% of the maternal dose." That’s a good sign. Some drugs are barely detectable in milk - like certain antidepressants or blood pressure meds. Others, like chemotherapy drugs, might show up in high amounts. The label will say if there are reports of drowsiness, poor feeding, or other side effects in breastfed infants. If it says "no adverse effects reported," that’s reassuring - but only if the data comes from a decent number of mothers. If it says "limited data," then proceed with caution.
Some labels even give you the actual concentration in milk: "peak milk concentration of 0.8 mg/L, 2 hours after maternal dose." That’s technical, but it tells you when the baby is most exposed. If you’re worried, you can time your dose right after feeding so the next feeding has the lowest amount.
Reproductive Potential Section (8.3)
This part isn’t just for women. It’s for anyone who could get pregnant or get someone pregnant. It tells you:- Do you need a pregnancy test before starting this drug?
- What kind of birth control is required? And what’s the failure rate of that method?
- Is there a risk of infertility? For men or women?
For example, some acne medications or MS drugs require two forms of birth control because they’re known to cause serious birth defects. The label will tell you exactly what’s needed - not just "use contraception," but "use two reliable methods with a combined failure rate under 1%." That’s specific. That’s helpful.
Why the New System Is Better - And Harder
The old letter system made things seem black and white. The new one shows you the gray. And that’s good. But it’s also harder. A 2018 study found 62% of obstetricians struggled with the new format at first. Why? Because you can’t scan a label and say "C - avoid." Now you have to read, think, and compare.But here’s the win: Misinterpretation dropped from 68% to 31%. That means fewer people are wrongly assuming a drug is dangerous when it’s not - or vice versa. The FDA now tracks over 25,000 pregnancies annually through mandatory registries. That’s more than four times the number before 2015. More data means better decisions down the line.
What to Do When You’re Not Sure
You don’t have to be an expert to use this. Here’s what works:- Ask your doctor: "Can you show me the Pregnancy and Lactation section for this drug?" Most have it open on their screen.
- Use trusted resources like MotherToBaby or TERIS. These are free, evidence-based services staffed by specialists who read these labels daily.
- If you’re on a chronic medication - like for epilepsy, depression, or high blood pressure - don’t stop it without talking to your provider. The risks of uncontrolled illness during pregnancy can be higher than the risks of the drug.
- Pharmacists are your allies. A 2021 survey showed 78% of pharmacists now spend 5-7 extra minutes counseling patients on these labels. Ask them.
What’s Changing in 2026?
The FDA is working on visual aids - simple icons that show risk levels at a glance. By 2025, they plan to update every pregnancy-related drug label. They’re also pushing for better data from diverse populations. Right now, only 15% of pregnancy registry participants are Black or Hispanic, even though those groups make up 30% of U.S. pregnancies. That gap matters.For now, the best tool you have is understanding what’s on the label. The information is there. You just need to know where to look - and what to ask for.
Are the old pregnancy letter categories (A, B, C, D, X) still used today?
No. The FDA officially replaced the letter categories with the Pregnancy and Lactation Labeling Rule (PLLR) in 2015. All new drug labels since then use narrative descriptions. Labels for older drugs were required to be updated by 2020. You may still see the letters on outdated packaging or websites, but they’re no longer official or accurate.
What does "infant exposure less than 10% of maternal dose" mean?
It means that when a mother takes a drug, only a small amount - less than 10% - passes into her breast milk. The baby then absorbs that small amount. For most drugs, exposure below 10% is considered low risk. For comparison, some medications may expose the baby to less than 1%, which is considered very low. This number helps you compare drugs - a drug with 2% exposure is likely safer than one with 8%.
If a drug says "risk cannot be ruled out," is it unsafe?
Not necessarily. "Risk cannot be ruled out" means there isn’t enough human data to say it’s safe - but it doesn’t mean it’s harmful. Many common drugs fall into this category, including some antibiotics and antidepressants. The key is to look at the actual numbers in the Risk Summary. If the background risk of birth defects is 3% and the drug shows no increase, then the risk is likely very low. The label gives you context - you just need to read it.
Can I trust drug labels from other countries?
The U.S. FDA’s PLLR is now the global standard. The European Medicines Agency (EMA) adopted a nearly identical system in 2016. So labels from the U.S., Canada, the EU, Australia, and other major markets are aligned. Labels from countries without strong regulatory oversight may still use outdated systems. Always check the source - if it’s from a national health authority like Health Canada or the TGA, it’s reliable. If it’s from a random website or pharmacy, verify it against the FDA’s official label.
What should I do if my doctor says a drug is safe but the label says "limited data"?
Ask for clarification. "Limited data" means there aren’t enough studies to be certain - not that it’s dangerous. Your doctor may be relying on clinical experience, expert guidelines, or data from similar drugs. Ask: "Is this based on studies in pregnant women, or is it an educated guess?" If the drug is essential for your health - like for epilepsy or severe depression - the benefit may outweigh the unknown risk. Always discuss alternatives, but don’t assume "limited data" means "avoid."
Where can I find the official FDA labeling for a drug?
Go to the FDA’s Drugs@FDA database at [email protected]. Search by brand or generic name. Click on the "Labeling" tab. You’ll see the full prescribing information, including Sections 8.1, 8.2, and 8.3. This is the official source - not the pharmacy website or drug company marketing material. Always check here if you’re unsure.


Amy Le
January 5, 2026 AT 13:36The FDA finally got something right. Those old A-B-C-D-X labels were infantile - like grading a nuclear reactor with a smiley face. Now we get real data. Real numbers. Real context. 🙌 No more guessing. No more panic. Just facts. And if your doctor still uses the old letters? Fire them. 🚫💊
Pavan Vora
January 6, 2026 AT 16:27Very nice explanation, but i think in india, most doctors still use old system... i saw a gynecologist yesterday, she said 'Category B, so safe'... i showed her the new label, she looked confused 😅 maybe we need more awareness? 🇮🇳
Indra Triawan
January 8, 2026 AT 12:13I just cried reading this. After my miscarriage, I was told 'it's probably just bad luck'... but what if it was the meds? I didn't know how to read any of this. I wish someone had explained this to me before I got pregnant. I'm not mad, just... heartbroken that this info wasn't easier to find.
Susan Arlene
January 10, 2026 AT 08:35so like... instead of one letter they give you a whole essay? cool. now i get why my doc just says 'take it' and moves on 😅
Joann Absi
January 10, 2026 AT 12:45THIS IS WHY AMERICA LEADS. 🇺🇸 The FDA didn’t just update a label - they upgraded human dignity. Meanwhile, other countries are still using medieval codes. We’re not just giving info - we’re giving POWER. And if you’re still using 'Category C' in 2026? You’re literally endangering lives. 😤
Ashley S
January 11, 2026 AT 16:45Why make it so hard? Just say 'safe' or 'dangerous'. People don't want to read paragraphs. They want a simple answer. This is just overcomplicating things. 🙄
Katelyn Slack
January 12, 2026 AT 00:12thank you for this. i showed this to my ob-gyn and she actually pulled up the FDA label on her tablet and walked me through it. i didn't know i could ask for that. i feel so much better now. 💙
Kiran Plaha
January 13, 2026 AT 00:25so if the label says 'limited data' but my doctor says it's fine, should i still worry? i'm 6 weeks and already stressed. just want to know if i'm being dumb or if this is normal.