Understanding Urinary Incontinence
Before we dive into addressing urinary incontinence following head surgery or trauma, it's essential to understand what this condition entails. Urinary incontinence is a common side effect of head trauma or surgery, where the individual struggles with controlling their bladder. It can manifest in various forms, including stress incontinence, urge incontinence, overflow incontinence, or functional incontinence. Depending on the severity of the head trauma or surgery, the type and degree of incontinence can vary considerably.
Identifying the Link Between Head Trauma and Urinary Incontinence
The brain is the control center of our body, managing everything from our thoughts to our bodily functions. Thus, any damage to the brain, either through injury or surgery, can potentially disrupt these functions. In the case of urinary incontinence, it's typically due to the brain's inability to correctly communicate with the bladder. This can result from injuries to the areas of the brain responsible for bladder control or damage to the nerves that carry signals between the brain and bladder.
Effects of Urinary Incontinence on Quality of Life
Urinary incontinence can significantly impact a person's quality of life. It's not just the physical discomfort, but also the emotional stress of dealing with unexpected leaks. People with urinary incontinence may feel embarrassed, leading to social isolation. Furthermore, they may have sleep disturbances due to frequent nighttime urination, impacting their overall health and wellbeing. Hence, it's crucial to address this problem effectively.
Initial Steps to Manage Urinary Incontinence
The first step to managing urinary incontinence is to consult a healthcare professional who can provide a proper diagnosis and treatment plan. This often involves a thorough examination, including neurological tests, to ascertain the extent of brain damage. In some cases, bladder control may improve as the brain heals, while in others, it may require specific treatment strategies.
Pelvic Floor Exercises and Bladder Training
One of the most effective ways to improve bladder control is through pelvic floor exercises and bladder training. These exercises strengthen the muscles that support the bladder, improving its ability to hold urine. Bladder training involves scheduling bathroom visits and gradually increasing the time between them, helping the bladder to hold more urine for longer periods.
Medications for Urinary Incontinence
In some cases, medications may be necessary to manage urinary incontinence. These work by either calming an overactive bladder or by blocking the signals that cause involuntary bladder contractions. However, it's essential to note that medications should always be taken under medical supervision, as they can have side effects.
Biofeedback and Electrical Stimulation
Biofeedback and electrical stimulation are other treatment options for urinary incontinence. Biofeedback uses sensors to track the bladder and sphincter muscles' activity, providing visual or auditory feedback to help you understand and control these muscles better. On the other hand, electrical stimulation involves sending mild electrical signals to the nerves controlling the bladder to improve their function.
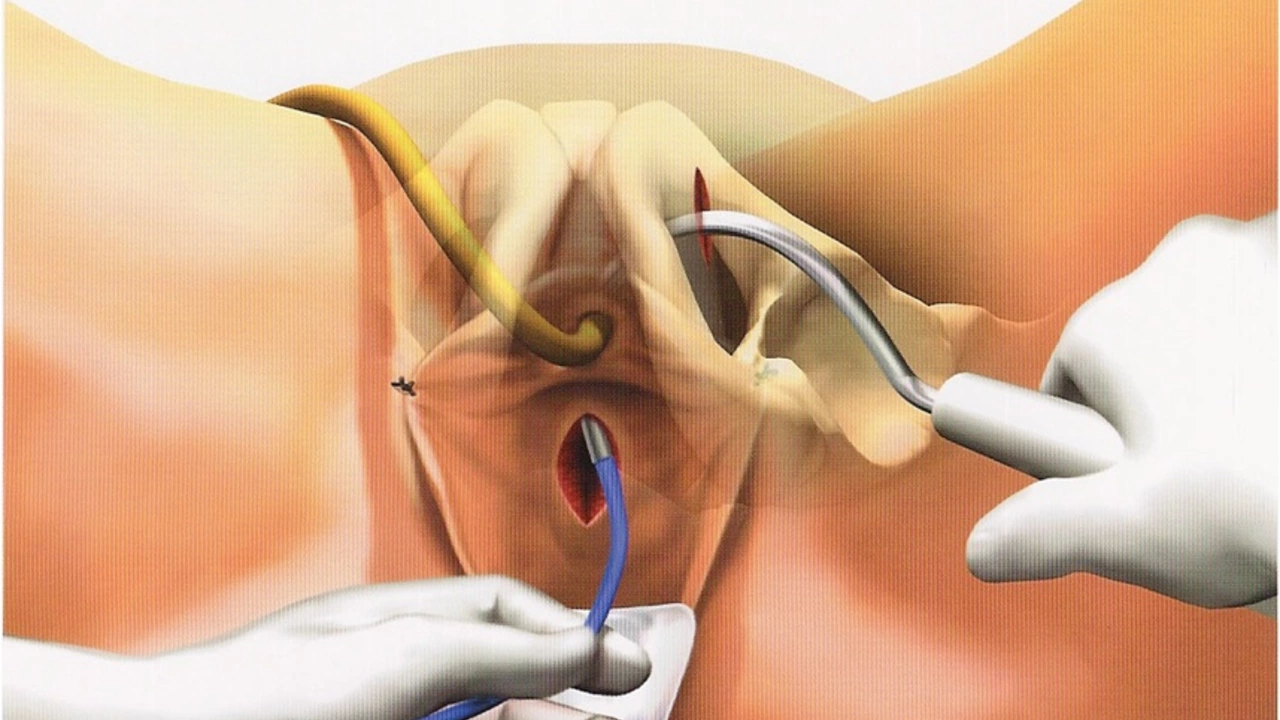
Advanced Treatment Options: Surgery and Neuromodulation
For severe cases of urinary incontinence that don't respond to other treatments, surgery or neuromodulation may be considered. Surgery can help improve bladder control by supporting the bladder or by increasing its capacity. Neuromodulation involves implanting a device that sends electrical signals to the nerves controlling the bladder, improving their function.
Managing Urinary Incontinence with Lifestyle Changes
Besides medical treatments, lifestyle changes can also support managing urinary incontinence. This can involve maintaining a healthy weight, avoiding bladder irritants like caffeine and alcohol, and drinking an adequate amount of water to prevent constipation, which can worsen incontinence.
Psychological Support for Urinary Incontinence
Lastly, it's crucial to remember that urinary incontinence can take a toll on mental health. It's not uncommon for individuals to experience anxiety, depression, or emotional distress. Therefore, psychological support, whether it's from a mental health professional, support groups, or loved ones, can be incredibly helpful in this journey.

peter richardson
July 26, 2023 AT 22:55Turns out he was leaking urine for weeks before anyone connected it to the brain surgery.
Dylan Kane
July 27, 2023 AT 05:42Lugene Blair
July 28, 2023 AT 03:36William Cuthbertson
July 28, 2023 AT 04:57We fix the body, but forget the soul that inhabits it.
Cosmas Opurum
July 29, 2023 AT 03:07Kirk Elifson
July 29, 2023 AT 10:23Shanice Alethia
July 29, 2023 AT 11:48Sam Tyler
July 29, 2023 AT 13:41Milind Caspar
July 30, 2023 AT 05:56shridhar shanbhag
July 30, 2023 AT 21:53John Dumproff
July 31, 2023 AT 05:17Hudson Owen
July 31, 2023 AT 06:09Steven Shu
July 31, 2023 AT 20:28Rose Macaulay
August 1, 2023 AT 14:59Ellen Frida
August 2, 2023 AT 05:21Sam Tyler
August 2, 2023 AT 14:53