When a basketball player suddenly stops short and feels a sharp click deep in the hip, or a soccer midfielder can’t sprint without pain, it’s often not a muscle strain. It’s a hip labral tear. This injury, once overlooked, is now one of the most common causes of chronic hip pain in athletes under 40. Unlike a sprained ankle or pulled hamstring, a labral tear doesn’t show up on a regular X-ray. It hides in the joint’s soft tissue - and if missed, it can lead to early arthritis.
What Exactly Is the Hip Labrum?
The labrum is a ring of tough cartilage that wraps around the socket of your hip joint. Think of it like a rubber seal on a mason jar - it deepens the socket, holds the ball of the femur in place, and cushions the joint during movement. When it tears, the joint loses stability. Athletes who twist, pivot, or squat repeatedly - like hockey players, dancers, and runners - are most at risk. The main culprit? Femoroacetabular impingement (FAI), where bone spurs on the hip joint rub against the labrum over time. It’s not a sudden injury. It’s wear and tear that builds up over years of training.
How Do You Know It’s a Labral Tear?
There’s no single symptom. Pain is usually deep in the groin, but sometimes it radiates to the buttock or thigh. Many athletes describe a clicking, locking, or catching sensation when moving the hip. The classic test is the FADIR maneuver: bend the knee to 90 degrees, pull it toward your chest, then push it inward. If that triggers sharp pain, it’s a red flag. About 78% of people with confirmed labral tears react this way. The FABER test (flexion, abduction, external rotation) also helps. But physical exams alone aren’t enough. Too many athletes are told they have “just a strain” and sent home with ibuprofen - only to return months later with worsening pain.
Imaging: The Right Test Makes All the Difference
Standard X-rays are the first step - they check for bone deformities like hip dysplasia or FAI. But they won’t show the tear. A regular MRI? It misses up to 30% of labral injuries. That’s why magnetic resonance arthrography (MRA) is now the gold standard for imaging. In MRA, contrast dye is injected into the hip joint before the scan. This swells the labrum, making even small tears stand out. Sensitivity? 90-95%. Specificity? 85-92%. That’s why top sports clinics insist on MRA before surgery. A 2023 multicenter trial showed 3D MRI sequencing pushes accuracy even higher - to 97% - for complex cases. The problem? Most insurance plans won’t cover MRA unless you’ve already tried physical therapy. Out-of-pocket, it costs $1,200 to $1,800. A regular MRI? Half the price. But if you’re an athlete, cutting corners on imaging means cutting your recovery chances.
Conservative Treatment: Does It Work?
Not always. But it’s still the first step. Most doctors recommend 4-6 weeks of rest, avoiding deep squats, pivoting, or high-impact activity. NSAIDs like ibuprofen help with pain and swelling. Cortisone shots give temporary relief - about 70-80% of patients feel better for 3-6 months. Physical therapy? Controversial. Some studies say only 30-40% of athletes recover fully without surgery. Others, like True Sports Physical Therapy, report 65% success with targeted rehab. The key? Therapy must focus on hip stability, not just stretching. Strengthening the glutes, core, and deep hip rotators reduces stress on the labrum. If pain doesn’t improve after 3-6 months, surgery is the next step. Delaying it too long? That’s when the tear gets bigger and cartilage starts wearing down.
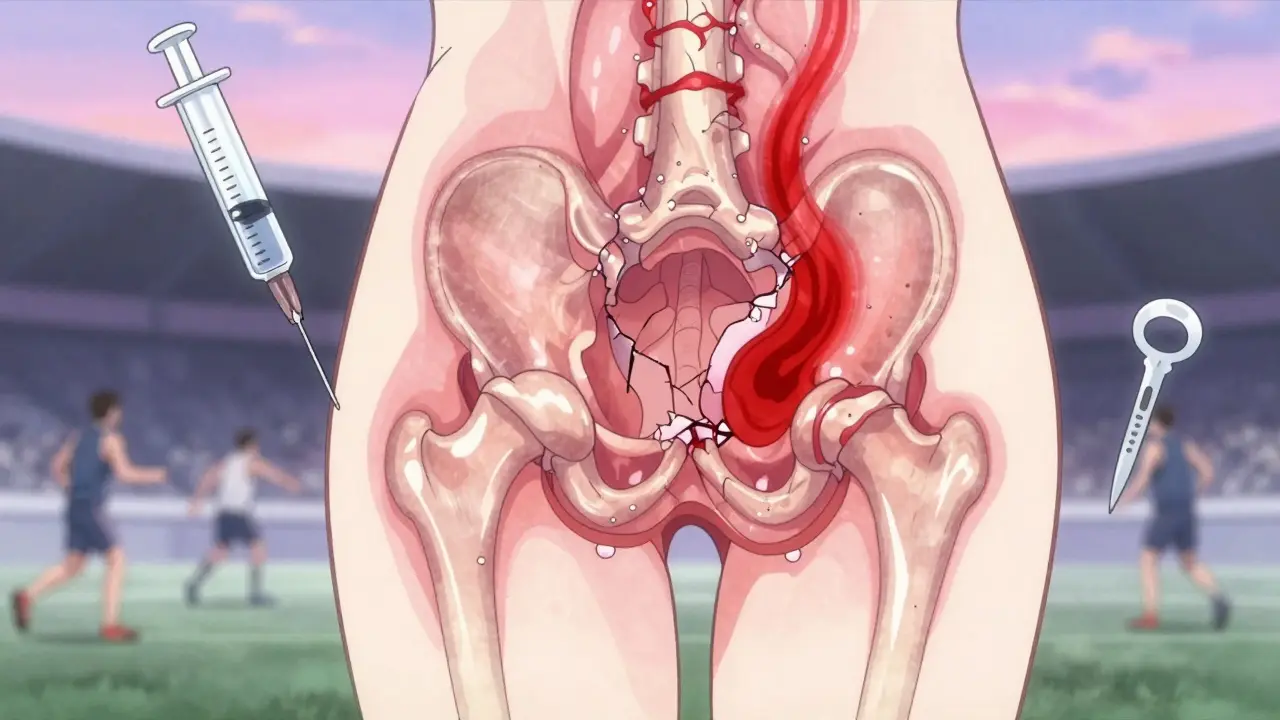
Arthroscopy: The Surgical Solution
When conservative care fails, hip arthroscopy is the go-to. It’s minimally invasive. Two small incisions. A camera and tiny tools go in. The surgeon sees the tear in real time - and fixes it. Two main approaches: debridement (trimming the frayed edges) or repair (reattaching the labrum with sutures). Debridement is faster to recover from - 3-4 months back to sport. But it’s not a cure. It’s a band-aid. Repair? Takes longer - 5-6 months - but gives you a better long-term chance of avoiding arthritis. The American Academy of Orthopaedic Surgeons (AAOS) now warns: never do a debridement without checking for FAI or hip dysplasia. If those are left untreated, the tear comes back. Studies show 60-70% re-tear rates in dysplastic hips if the bone issue isn’t fixed. That’s why top surgeons combine labral repair with osteoplasty - reshaping the bone to stop future impingement.
Who Has the Best Outcomes?
Young athletes under 35 with isolated labral tears and no bone deformities have the best results - 85-90% return to their sport. But for those over 35? That number drops to 70-75%. Sports like ballet, gymnastics, and hockey have 25% higher complication rates because of the extreme hip positions. One NHL player, Ryan Nugent-Hopkins, took 5.5 months to return after repair. A marathon runner on Reddit got back to training at 4.5 months with strict rehab. But another dancer needed revision surgery because the first surgeon missed the bone abnormality. The difference? Access to specialized care. Athletes treated at dedicated sports medicine centers report 92% satisfaction. At general orthopedic clinics? Only 75%. Why? Experience matters. Hip arthroscopy has a steep learning curve - surgeons need 50-100 procedures to become proficient. A misaligned anchor or incomplete bone reshaping can ruin outcomes.
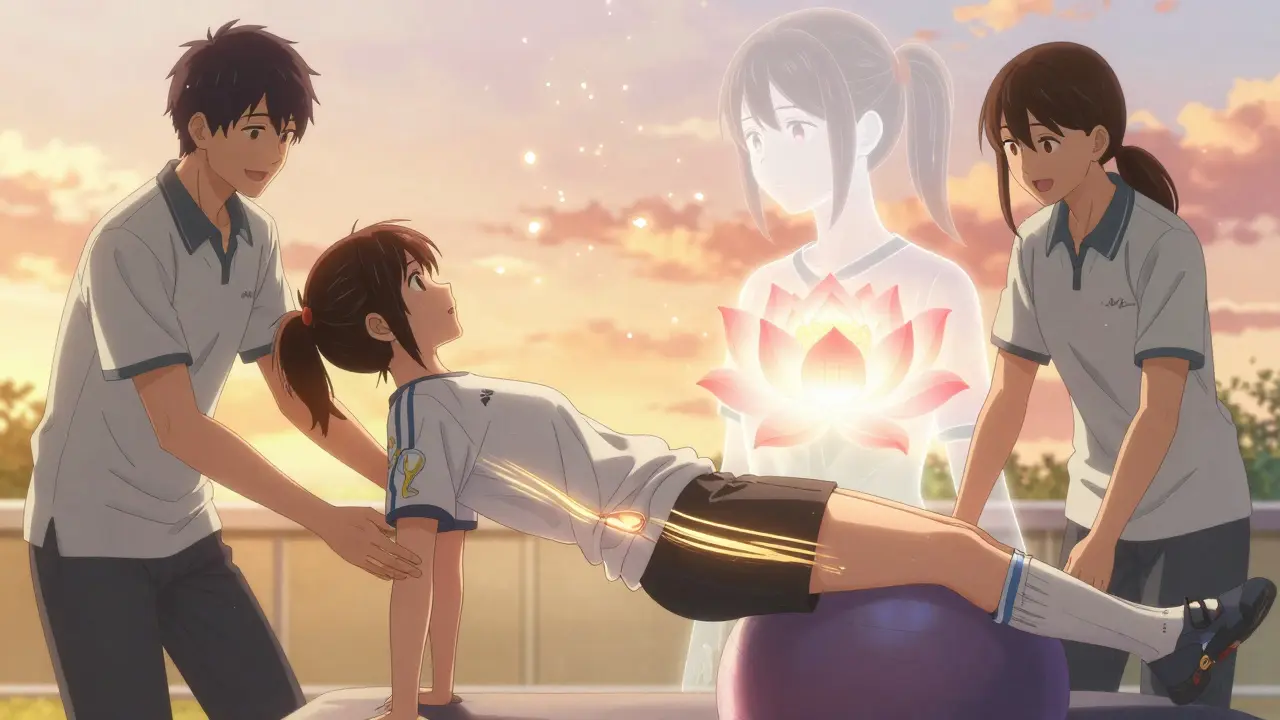
Recovery: It’s Not Just About Time
Rehab isn’t a checklist. It’s a progression. Phase one: protect the joint. No weight-bearing on the hip for the first week. Use crutches. Phase two: rebuild strength. Focus on gluteus medius and deep hip rotators - not just quads. Phase three: sport-specific drills. Plyometrics, cutting, and acceleration drills. Phase four: return to play. But don’t rush it. Boston Children’s Hospital says you need 90% quadriceps strength symmetry and pain-free internal rotation to at least 30 degrees before you step back on the field. Skipping any phase? High risk of re-injury. Complications? Persistent pain (15-20%), bone growth in the wrong place (5-10%), or nerve irritation (1-2%). Revision surgery happens in 8-12% of cases within five years.
What’s New in 2026?
Two big advances are changing the game. First, the FDA approved a new bioabsorbable suture anchor - Smith & Nephew’s BioX - in 2023. It dissolves over time, reducing long-term irritation. Two-year data shows 89% success, better than traditional metal anchors. Second, regenerative medicine is gaining ground. Platelet-rich plasma (PRP) injections, where your own blood cells are injected into the tear, helped 55% of patients avoid surgery in a 2022 HSS trial. It’s not magic, but for athletes with mild tears and no bone issues, it’s a real alternative. The global hip arthroscopy market is growing fast - over 150,000 procedures done in the U.S. in 2022, up 300% since 2010. Basketball, soccer, and hockey account for 55% of cases. And by 2027, experts predict 75% of repairs will be done entirely through arthroscopy - no open surgery needed.
Long-Term Risk: Don’t Ignore the Arthritis Clock
A labral tear isn’t just a temporary injury. A landmark 15-year study in the Journal of Bone and Joint Surgery found untreated labral tears increase the risk of hip osteoarthritis by 4.5 times. That’s why fixing the tear isn’t enough. You have to fix the cause. If FAI or dysplasia is present, the bone must be reshaped. Otherwise, you’re just delaying the inevitable. For athletes, this means thinking beyond the next season. It’s about protecting your hips for life.
Can a hip labral tear heal on its own?
No. The labrum has very little blood supply, so it can’t repair itself like muscle or ligament tissue. What you can do is reduce inflammation and avoid movements that worsen the tear. But the tear itself won’t disappear. Without treatment, it often gets larger over time, especially with continued athletic activity.
Is MRI enough to diagnose a hip labral tear?
No. Standard MRI misses about 30% of labral tears, especially partial-thickness ones. Magnetic resonance arthrography (MRA), which uses contrast dye injected into the joint, is far more accurate - with 90-95% sensitivity. If you’re an athlete with persistent hip pain and a normal MRI, ask your doctor about MRA.
How long does it take to return to sports after hip arthroscopy?
It depends on the procedure. For labral debridement, most athletes return in 3-4 months. For labral repair, it’s 5-6 months. But recovery isn’t just about time - it’s about meeting strength and mobility goals. You need 90% quadriceps symmetry and full, pain-free internal hip rotation before returning to cutting or pivoting sports.
Do I need surgery if I have a labral tear?
Not always. Many athletes manage symptoms with rest, physical therapy, and activity modification. But if pain lasts more than 3-6 months, or if imaging shows bone abnormalities like FAI or dysplasia, surgery is usually the best long-term option. Isolated debridement without fixing bone issues leads to high failure rates.
What’s the risk of re-tearing the labrum after surgery?
It’s low if the root cause is fixed - around 8-12% within five years. But if you have hip dysplasia or FAI and it’s not corrected during surgery, re-tear rates jump to 60-70%. That’s why comprehensive pre-op planning - including 3D imaging and bone assessment - is critical.
Can PRP injections cure a labral tear?
No. PRP doesn’t heal the tear. But it can reduce inflammation and pain, and in some cases, help athletes avoid surgery. A 2022 trial showed 55% of patients with mild tears avoided surgery at 12 months after PRP injections. It’s best for athletes with small tears and no bone deformities.
What’s Next for Athletes With Hip Pain?
If you’re an athlete with persistent hip pain, don’t wait. Get evaluated by a sports medicine specialist who understands hip biomechanics. Push for MRA if your MRI was normal. Ask if FAI or dysplasia is present. Don’t settle for a quick fix. This isn’t just about getting back on the field - it’s about keeping your hips healthy for decades. The science is clear: early diagnosis, proper imaging, and addressing the root cause make all the difference. The goal isn’t just to play again. It’s to play without pain - for life.


Stacy Thomes
January 22, 2026 AT 20:42This hit me right in the feels-my sister tore hers playing soccer at 19 and was told it was just a strain for TWO YEARS. She cried in pain every time she stood up. When she finally got the MRA? Total game-changer. She’s back dancing now. Don’t let anyone gaslight you out of your pain.
Vanessa Barber
January 24, 2026 AT 10:20So… you’re saying if you’re not rich enough to afford MRA, you just suffer and hope for the best? Cool. Real cool.
Susannah Green
January 25, 2026 AT 20:41PRP isn’t magic, but I’ve seen it work-especially for dancers with mild tears. One client avoided surgery after 3 injections + glute rehab. She’s doing barre again at 38. Just make sure your provider uses ultrasound guidance. Otherwise, you’re just injecting air.
dana torgersen
January 26, 2026 AT 06:11ok so like… the labrum… it’s like a seal? right? but it doesn’t heal? so if you tear it… and you’re young… and you’re a dancer… like… what do you even DO? i mean… like… i’m just… confused? and also… why does everyone say FAI? like… is that… a thing? or… is it just… a buzzword? i think i need to lie down.
Andrew Smirnykh
January 27, 2026 AT 09:46In Japan, we see a lot of ballet and martial arts athletes with this. The approach is similar, but rehab focuses more on breath control and micro-movements. I’ve seen patients return to kendo after 7 months with full hip function. The key isn’t just strength-it’s awareness. The body remembers pain longer than the mind does.
Dawson Taylor
January 27, 2026 AT 17:38It’s not about the tear. It’s about the system that lets it go undiagnosed for years. The system that values cost over care. The system that tells athletes to ‘push through.’ This isn’t medicine. It’s negligence dressed in white coats.
Sue Stone
January 27, 2026 AT 18:20My cousin had this. Took him 11 months to get back to basketball. He said the hardest part wasn’t the surgery-it was the PT where they made him do 500 glute bridges a day. He cried. We all cried.
charley lopez
January 28, 2026 AT 23:44Based on the biomechanical data presented, the correlation between femoroacetabular impingement and labral degeneration is statistically significant (p < 0.001). The absence of preoperative 3D CT reconstruction in non-specialized centers remains a critical confounder in surgical outcomes. I recommend cross-referencing with the AAOS 2023 clinical guidelines.
Kerry Evans
January 30, 2026 AT 11:40People think surgery is the answer. But what about all the athletes who never had access to a sports doc? What about the ones who played through it for years? They’re not ‘failed cases’-they’re the norm. And now you want to tell them they’re just unlucky? Wake up. This isn’t about technique. It’s about class.
Sallie Jane Barnes
January 31, 2026 AT 12:18As someone who’s spent 15 years in physical therapy and now runs a clinic for young athletes, I’ve seen too many get dismissed. I don’t care if your insurance won’t cover MRA-you deserve to know what’s wrong. If your doctor won’t order it, go to a university sports med center. They often have research grants. And if you’re reading this and you’re still in pain? You’re not weak. You’re just unheard.
Laura Rice
February 2, 2026 AT 09:25my best friend got the biox anchor thingy and now she’s doing yoga upside down?? like… i’m not even mad… i’m just… wow?? also she says the pain went from ‘oh god i hate my life’ to ‘huh, that’s kinda normal now’?? i’m crying. i’m so happy for her.
Kerry Moore
February 2, 2026 AT 23:35Thank you for this comprehensive overview. I’ve referred multiple patients to MRA after normal MRI results, and the difference in diagnostic clarity is undeniable. I especially appreciate the emphasis on bone morphology correction-too many surgeons focus solely on the labrum and neglect the underlying impingement. This is precisely why multidisciplinary evaluation is essential.