When you're making medical devices, precision isn't optional. A thermometer off by half a degree, a scale that reads 2 grams too high, or a pressure sensor drifting over time-these aren't just minor errors. They can mean a patient gets the wrong dose, a implant fails in surgery, or a whole batch of products gets recalled. That’s why equipment calibration and validation aren’t just paperwork. They’re the backbone of quality in manufacturing.
What’s the Difference Between Calibration and Validation?
People mix these up all the time. Calibration is about accuracy. It’s checking if your device reads the same as a known standard. If your digital scale says 100 grams when you put a 100-gram weight on it, it’s calibrated. If it says 102 grams? It’s out of tolerance. Calibration makes sure your instrument matches reality.
Validation is about performance. It asks: does this machine do what it’s supposed to do in real-world conditions? For example, a sterilizer might be perfectly calibrated to hit 121°C-but validation proves it kills all bacteria in a full load, even when the door is opened mid-cycle. Validation doesn’t care if the thermometer is accurate. It cares if the whole process works.
Think of it this way: calibration checks the ruler. Validation checks if the house you built with that ruler is safe to live in.
Why ISO 13485:2016 Is the Gold Standard
If you’re making medical devices, ISO 13485:2016 is your rulebook. It doesn’t say "calibrate sometimes." It says: every measuring device must be calibrated at specified intervals or before use. And those intervals? They can’t be guesswork. You need proof.
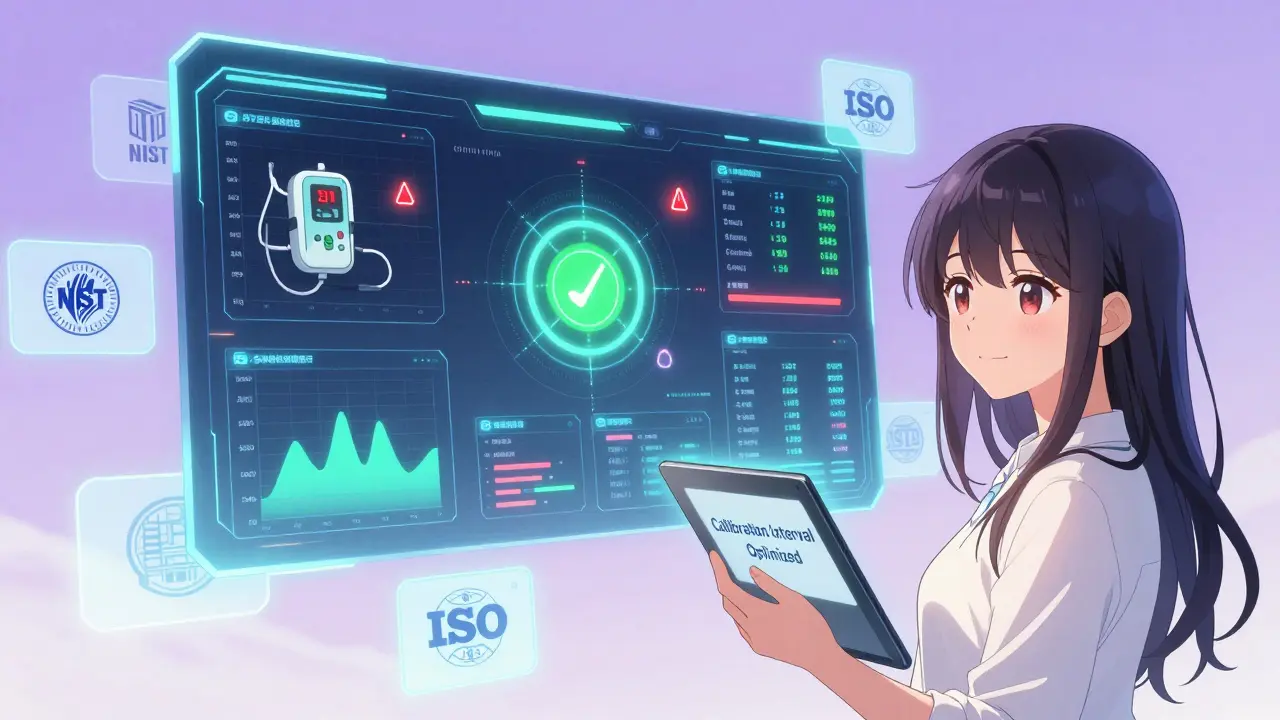
The standard requires traceability to the International System of Units (SI). That means your calibration standard must link back-through a documented chain-to a national lab like NIST in the U.S. or NMI in Australia. No shortcuts. No "it was good last time." Each step has to be recorded with uncertainty values. If your calibration certificate doesn’t show measurement uncertainty, it’s not compliant.
And here’s the kicker: the uncertainty of your calibration must be less than 25% of the tolerance you’re trying to measure. So if your device must hold ±0.1 mm, your calibration standard must be accurate to ±0.025 mm or better. Most companies miss this. They focus on the reading, not the math behind it.
Calibration Intervals: One Size Doesn’t Fit All
Manufacturers often give you a recommended interval-say, every 6 months. But ISO 9001 and ISO 13485 let you adjust that based on risk and history. The trick is proving it.
Here’s how a smart shop does it:
- Start with the manufacturer’s recommendation.
- Track every calibration result for 12-24 months.
- If the device stays within tolerance every time? Extend the interval.
- If it drifts after 3 months? Shorten it.
One medical device maker in Adelaide cut calibration frequency for their precision micrometers from quarterly to biannually after collecting 18 months of data. Saved $18,500 a year. No audits failed. No products rejected.
But don’t get lazy. High-risk tools-like those measuring drug dosages or implant dimensions-often need monthly checks. Basic tools, like a simple ruler used only for labeling, might only need annual calibration. Risk-based scheduling isn’t cutting corners. It’s smart resource use.
Environmental Factors Are Silent Killers
Calibrating a device at 20°C and 40% RH? Great. Now put it in a factory where it’s 32°C and 80% humidity. That device will drift. Fast.
NIST found that 57.8% of out-of-tolerance events happen when temperature swings more than ±5°C from calibration conditions. Humidity? Even worse for electronics and sensors.
Companies in humid climates like Brisbane or Singapore see pH meters, moisture analyzers, and electronic balances fail more often. The fix? Control the environment. Install climate-controlled rooms for critical equipment. Or-better yet-calibrate the device where it’s used. Not in a lab 100 meters away. Right where it lives.
Validation: The Three-Step Process
Validation isn’t a one-time event. It’s a process. GAMP 5 breaks it down into three phases:
- Installation Qualification (IQ): Did you install the equipment right? Are all parts there? Are manuals and software versions correct?
- Operational Qualification (OQ): Does it work under all conditions? Test extremes-max speed, min temperature, full load, empty load. Run it until it breaks. Document everything.
- Performance Qualification (PQ): Does it produce consistent results with real product? Run 3 consecutive batches. Test output. Compare to specs.
Validation for a simple labeling machine might take 2 weeks. For a robotic arm that welds pacemaker housings? Six months. Costs range from $25,000 to half a million. But skipping it? That’s a $5 million recall waiting to happen.
Digital Tools Are Changing the Game
Spending 15 hours a week chasing down calibration certificates? You’re not alone. 58.3% of small manufacturers say documentation is their biggest headache.
Cloud-based calibration software like GageList or Trescal automates the whole thing. They track due dates, send reminders, store certificates digitally, and generate audit-ready reports in seconds. Companies using these tools cut audit prep time by over 60%.
Even better: some are using IoT sensors on equipment to monitor real-time performance. If a laser cutter starts drifting, the system flags it before the next scheduled calibration. One company reduced calibration frequency by 40% without a single failure. That’s risk-based maintenance in action.
The Hidden Cost of Non-Compliance
FDA warning letters in 2023 cited inadequate calibration in 37.2% of cases. That’s more than poor documentation, more than untrained staff. It’s the #1 reason for production halts and recalls.
Small manufacturers (<50 employees) pay 22.3% more per device to stay compliant. Why? They can’t negotiate bulk discounts with calibration labs. They don’t have in-house metrologists. They’re forced to outsource everything-and pay premium rates.
But here’s the flip side: investing in calibration software, training, and environmental controls pays back fast. One mid-sized manufacturer in Melbourne reduced non-conformances by 27% after adopting SAE AS9100D’s Method 5 for interval planning. Their audit score jumped from 78% to 96% in one year.
What’s Coming Next?
ISO 13485:2016 was amended in March 2024 to require continuous validation for AI-driven measurement systems. If you’re using machine learning to predict defects or adjust production in real time? You now need to validate the algorithm’s drift over time-not just the sensor.
The FDA’s 2024 Calibration Modernization Initiative demands all Class II and III device manufacturers switch to electronic records by December 31, 2026. Paper logs are officially outdated. If you’re still using Excel spreadsheets and printed certificates, you’re already behind.
And in the background? NIST is developing quantum-based standards that could make electrical measurements 100 times more accurate by 2030. That means future calibrations could be done remotely, with near-zero uncertainty.
Where to Start
If you’re new to this, don’t try to fix everything at once. Start here:
- Inventory every measuring device. List it. Give it a unique ID.
- Classify by risk: critical, important, basic.
- For critical devices, establish traceable calibration with documented uncertainty.
- Start collecting calibration data for 6 months. Use it to justify intervals.
- Invest in one calibration management tool. Don’t wait for perfection.
Compliance isn’t about checking boxes. It’s about building trust-with regulators, customers, and patients. The right calibration and validation program doesn’t cost money. It saves it. And lives.


Lance Nickie
January 14, 2026 AT 11:47Clay .Haeber
January 14, 2026 AT 21:33Nelly Oruko
January 16, 2026 AT 00:01Angel Tiestos lopez
January 17, 2026 AT 07:22Scottie Baker
January 19, 2026 AT 02:55Anny Kaettano
January 19, 2026 AT 05:57Kimberly Mitchell
January 19, 2026 AT 12:55Rosalee Vanness
January 21, 2026 AT 00:16Lethabo Phalafala
January 21, 2026 AT 18:37Milla Masliy
January 23, 2026 AT 00:20Damario Brown
January 23, 2026 AT 15:05sam abas
January 23, 2026 AT 21:25John Pope
January 25, 2026 AT 05:22