Why so many people still don’t trust generic drugs
It’s 2026, and nearly 91% of prescriptions filled in the U.S. are for generic drugs. Yet, if you walk into a community clinic and ask patients why they refuse a generic prescription, you’ll hear the same things: "It won’t work like the brand," "I feel different on it," or "My doctor said the real one is better." These aren’t just myths-they’re deeply held beliefs, shaped by packaging, color changes, and years of marketing that made brand names feel like the only "real" medicine.
The truth? Generic drugs are not cheaper because they’re weaker. They’re cheaper because they don’t need to spend millions on ads or re-prove what’s already been proven. The FDA requires every generic to have the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. And they must prove it works the same way-within 80% to 125% of the brand’s performance in the body. That’s not a guess. That’s science, tested in clinical trials with thousands of patients.
How the FDA ensures generics work just as well
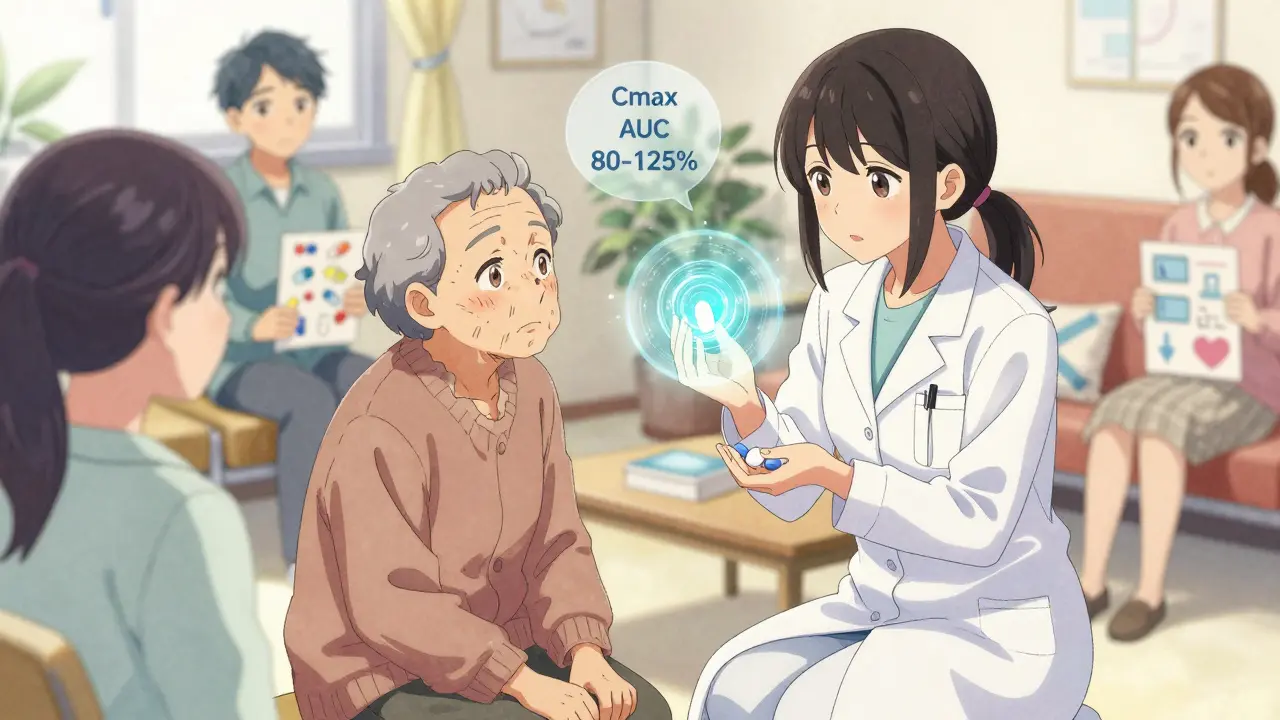
The FDA doesn’t just approve generics because a company says they’re the same. They demand proof. Every generic drug must pass a bioequivalence study, which measures how much of the drug enters the bloodstream and how fast. These studies look at two key numbers: Cmax (the highest concentration in the blood) and AUC (how much drug is absorbed over time). If the generic’s results fall within 80-125% of the brand’s, it’s approved. That’s a tight range-and it’s not just for pills. The same rules apply to patches, inhalers, and even complex topical creams.
Since 2012, the FDA has reviewed about 1,000 generic applications every year. In 2022, they hit their target: 90% of applications were reviewed within 10 months. That’s speed without cutting corners. And every batch of generic drug is inspected for quality, purity, and stability-just like the brand. The FDA doesn’t treat generics as second-class. They treat them as equal.
The real cost difference-and why it matters
On average, generic drugs cost 80-85% less than their brand-name counterparts. In 2022, that saved the U.S. healthcare system $377 billion. That’s not a rounding error. That’s enough to cover free prescriptions for millions of people who skip doses because they can’t afford their meds.
For someone managing high blood pressure, diabetes, or cholesterol, switching to a generic can mean the difference between taking their medicine every day or skipping it to pay for groceries. A 2021 study tracking 3.2 million patients found that when people switched to generics, their adherence improved by 22%. That’s not just savings-it’s fewer hospital visits, fewer complications, and longer lives.
And it’s not just low-income patients. Medicare beneficiaries, retirees on fixed incomes, and even those with insurance face high copays on brand-name drugs. The 2023 Consolidated Appropriations Act now requires all Medicare Part D plans to hand out standardized generic education materials by January 2025. Why? Because when people understand the value, they’re more likely to use it.
Why patients still hesitate-even when it’s safe
Here’s the strange part: pharmacists know generics work. A 2021 survey showed 97% of pharmacists have full confidence in them. But patients? Only about 52% accept generics unless their doctor specifically says, "This is just as good." That number jumps to 89% when a doctor recommends it outright. That’s the power of trusted voices.
But there are other reasons. Appearance matters. A patient might have taken a white oval pill for years, then get a blue round one and think, "This isn’t the same." In a University of Michigan survey, 23% of patients questioned whether their new pill was the right medicine just because it looked different. The FDA even has a fact sheet for this: "Color and shape don’t affect how the drug works." Then there’s the nocebo effect-the opposite of placebo. In one study, patients who were told they were switching to a generic reported more side effects-even though the pill was identical. When they didn’t know they were on a generic, side effects dropped. Belief can change how you feel.
What works in community health presentations
Community health centers aren’t just handing out brochures anymore. They’re using proven tools from the FDA’s Generic Drug Stakeholder Toolkit. The most effective method? The "Teach-Back" technique.
Instead of saying, "This is a generic version," they say:
- "The FDA requires this medicine to have the same active ingredient as the brand-name drug."
- "It works the same way in your body."
- "It’s been tested on thousands of people."
- "And it costs a lot less."
Then they ask: "Can you tell me in your own words why this medicine is safe?" If the patient can explain it back, they’ve understood. If not, they go over it again. This simple method increased patient acceptance by 37% in one Burlington clinic within six months.
They also use videos. The FDA’s "Generics 101" series, launched in 2023, is now playing in waiting rooms across the country. It’s short, clear, and made for older adults. Preliminary data shows viewers aged 65+ improved their knowledge retention by 31%.
When generics aren’t the obvious choice
Most of the time, generics are the right call. But there are exceptions. A 2023 study in Epilepsy & Behavior found that patients switching between generic and brand antiepileptic drugs had a slightly higher chance of seizure recurrence-12.7% more. That’s why neurologists often stick with the brand for epilepsy patients, especially those with unstable control.
But the American Academy of Neurology is clear: this is rare. They call it "an exception proving the rule." For 99% of other conditions-high blood pressure, cholesterol, asthma, depression, thyroid issues-generics are just as safe and effective.
The bigger issue isn’t the science. It’s access. Rural areas still lag behind cities. Only 78% of prescriptions filled in rural communities are generics, compared to 93% in urban areas. Why? Fewer pharmacists, less education, and sometimes, just less exposure to the message.
What’s next for generic drug education
The future of generic education is tied to equity. The National Association of Community Health Centers now requires all patient counseling sessions to include generic drug information-starting January 2024. Why? Because cost is a barrier to health, and generics remove that barrier.
More complex generics are coming too. Inhalers, injectables, and topical creams are harder to copy than pills. These need more detailed explanations. The FDA’s 2023 survey found patients were 40% more confused about these types. That means community health workers need better tools-and more training.
Meanwhile, the Association for Accessible Medicines has distributed 2.7 million brochures through over 14,000 health centers since early 2023. These aren’t just handouts. They’re conversation starters. They’re visual. They’re in English and Spanish. And they’re working.
What you can do right now
If you’re a patient: Ask your pharmacist or doctor, "Is there a generic version?" Don’t assume it’s not available. Ask why they’re prescribing the brand. If they say "It’s better," ask for the evidence. Most of the time, they’ll say, "It’s the same." If you’re a community health worker: Use the FDA’s free toolkit. Use the Teach-Back method. Show patients the color chart of pills. Play the "Generics 101" video. Make it simple. Make it real.
If you’re a prescriber: Say it clearly. "I’m prescribing this generic because it’s just as effective and will save you money. I’ve used it myself." The science is settled. The savings are real. The only thing left to change is the story we tell.
Are generic drugs really as safe as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they work the same way in the body through strict bioequivalence testing. Every generic is held to the same quality standards as the brand.
Why do generic pills look different from brand-name ones?
The appearance-color, shape, size-isn’t part of the drug’s effectiveness. It’s changed because manufacturers can’t copy the brand’s look due to trademark laws. But the active ingredient, how it’s absorbed, and how it works in your body are identical. The FDA confirms that differences in appearance do not affect safety or performance.
Do generics take longer to work than brand-name drugs?
No. Bioequivalence studies show that generics reach the same peak concentration in the blood at the same rate as brand-name drugs. Any difference in how quickly you feel the effect is usually due to your body’s response, not the drug itself.
Can I switch from a brand-name drug to a generic safely?
For most medications, yes. Over 90% of prescriptions in the U.S. are for generics, and they’re used safely every day. For a few drugs-like certain epilepsy medications-doctors may recommend staying on the brand due to very narrow dosing ranges. Always talk to your doctor before switching, but don’t assume the brand is safer.
Why do some people say they feel worse on generics?
This is often the nocebo effect-when you expect to feel worse, your brain interprets normal sensations as side effects. Studies show patients report more side effects when they know they’re taking a generic, even when the pill is identical. Once they’re blinded to what they’re taking, those reports drop. Talking openly with your provider can help reduce this fear.
Are generic drugs made in the same facilities as brand-name drugs?
Many are. The FDA inspects all manufacturing sites-whether for brand or generic-using the same standards. About half of all generic drugs are made in the same factories as the brand-name versions. The rest are made in facilities that meet the same quality rules. The FDA doesn’t allow lower standards just because it’s a generic.
How much money can I save by using generics?
On average, generics cost 80-85% less than brand-name drugs. For example, a 30-day supply of a brand-name blood pressure pill might cost $120, while the generic costs $15. That’s over $1,000 a year saved. In 2022, generics saved the U.S. healthcare system $377 billion total.
Do insurance plans cover generics better than brand-name drugs?
Yes. Most insurance plans have lower copays for generics. Some even require you to try the generic first before covering the brand. Medicare Part D plans are now required to provide generic education materials to all beneficiaries by January 2025, to help people understand their options and savings.
Is there a difference between generic drugs from different manufacturers?
All FDA-approved generics must meet the same bioequivalence standards, so they work the same way. Differences between manufacturers are usually in inactive ingredients (like fillers or dyes), which don’t affect how the drug works. If you notice a change in how you feel after switching between two generics, talk to your pharmacist-they can check if the inactive ingredients might be causing a reaction.
Where can I find reliable information about generic drugs?
The FDA’s website has a free library of over 2,147 educational resources, including videos, fact sheets, and toolkits for patients and providers. The Association for Accessible Medicines also offers free materials through community health centers. Always rely on official sources like the FDA, CDC, or your pharmacist-not social media or anecdotal stories.

Saumya Roy Chaudhuri
January 10, 2026 AT 02:54Oh my god I just had to comment because this is EVERYTHING. I’m from India and we’ve been using generics for decades-my grandmother took a generic blood pressure pill for 20 years and lived to 94. The color changed three times, the shape changed twice, and she never missed a dose. People in the US act like generics are some kind of experimental lab experiment. No. They’re the reason millions of people can afford to live. Stop romanticizing Big Pharma and start trusting science.
Ian Cheung
January 10, 2026 AT 22:03Bro I used to be one of those people who refused generics until my insulin bill went from $400 to $35. I cried in the pharmacy. Not because I was scared-I was just dumb. The pill looked different. Same box. Same script. Same damn results. Now I tell everyone: if your doctor says it’s the same, it’s the same. Stop paying for branding and start paying for health. 🙏
anthony martinez
January 11, 2026 AT 17:22Interesting how the FDA’s 80-125% bioequivalence range is treated like gospel when it’s literally a 45% window. That’s not precision. That’s a ballpark. And yet somehow, when it’s a brand-name drug, every molecule must be identical. But when it’s generic? Eh, close enough. I’m not saying generics are unsafe-I’m saying the narrative is oversimplified.
Mario Bros
January 12, 2026 AT 08:41Y’all need to stop overthinking this. I’m a nurse. I’ve seen people skip meds because they cost $120. I’ve seen people in ERs because they skipped meds. Generics save lives. Plain and simple. If your pill looks different, cool. That’s not the drug-that’s the packaging. Your body doesn’t care about the color. It cares about the dose. And if your doctor says it’s the same? Believe them. 💪
Jake Nunez
January 12, 2026 AT 16:59I grew up in rural Kentucky. We didn’t have a pharmacy with more than three aisles. The first time I saw a generic pill that wasn’t white and oval, I thought it was a mistake. Took me three visits to the clinic to finally ask, ‘Is this the same?’ The pharmacist didn’t even blink. Just handed me the FDA fact sheet. I’ve been on generics for six years now. My cholesterol’s down. My wallet’s happy. And I still don’t know why this is even a debate.
Christine Milne
January 13, 2026 AT 04:15While I appreciate the sentiment, this article exhibits a concerning degree of ideological bias. The FDA’s bioequivalence standard of 80-125% is statistically permissive and lacks the rigorous consistency demanded by the European Medicines Agency. Furthermore, the claim that generics are ‘just as safe’ is misleading when one considers the variance in inactive ingredients, which can trigger adverse reactions in sensitive populations. This is not a matter of trust-it is a matter of regulatory disparity and compromised pharmacological integrity.
Bradford Beardall
January 14, 2026 AT 17:31Wait-so if the FDA inspects the same factories for brand and generic, why do we still hear stories about generic manufacturers cutting corners? I’ve read reports about facilities in India and China with multiple warning letters. Is that just noise? Or are we pretending all generics come from spotless labs? The science says they work. But the supply chain? That’s a different story.
McCarthy Halverson
January 15, 2026 AT 21:41Generic works. Same pill. Same effect. Save money. Take it. No drama. If you feel weird, talk to your pharmacist. They’ll check the filler. That’s it.
Michael Marchio
January 16, 2026 AT 20:42Let’s be honest here. The reason people don’t trust generics isn’t because they’re misinformed-it’s because they’ve been lied to for decades. The pharmaceutical industry spent billions convincing us that brand equals quality. And now they’re trying to rebrand themselves as the ‘good guys’ because they’re losing money. The FDA’s approval process is a rubber stamp for corporate profit. They don’t test for long-term effects. They don’t test for interactions with other generics. They don’t test for psychological dependence on brand names. This isn’t science. It’s marketing dressed up as public health.
Jake Kelly
January 18, 2026 AT 06:16I just wanted to say thank you for writing this. My mom’s on six different meds. Half are generics. She used to stress about the color changes. Now she laughs about it. She says, ‘If it helps me breathe, I don’t care if it’s purple or blue.’ That’s the real win here-not the savings, not the science. It’s peace of mind.
Ashlee Montgomery
January 18, 2026 AT 08:26What’s interesting is how much of this is about identity. We don’t just take pills-we take stories. The brand-name pill is the one we were told was ‘real.’ The generic is the one we were told to settle for. But what if the real medicine was never the pill at all? What if it was the belief that we deserved to be healthy, regardless of cost? Maybe the real breakthrough isn’t in the chemistry-it’s in the narrative we choose to believe.
neeraj maor
January 18, 2026 AT 08:32Let me guess-the FDA is in bed with Big Pharma. The ‘bioequivalence’ range? A loophole. The ‘same factory’ claim? A lie. The ‘377 billion saved’? A PR stunt. They’re flooding the market with generics so they can phase out the brand-name drugs entirely and then jack up prices again on the next ‘new’ version. They’ve done it before. Look at insulin. Look at EpiPens. This isn’t about access-it’s about control. And the people who believe this ‘educational’ propaganda are the ones who’ll be paying the price later.