When you're in the middle of a panic attack, time doesn't just slow down-it feels like it stops. Your heart pounds, your chest tightens, and your mind races with thoughts you can't control. In those moments, a benzodiazepine can feel like a lifeline. It doesn't take long-sometimes just 30 minutes-for the fog to lift, the trembling to stop, and your breathing to return to normal. That's why these drugs became the go-to solution for acute anxiety, panic, and even seizures. But here's the catch: what helps you today might trap you tomorrow.
How Benzodiazepines Work
Benzodiazepines don't just make you feel calm-they change how your brain works at a chemical level. They boost the effect of a natural brain chemical called GABA, which acts like a brake pedal for overactive nerve cells. When those cells calm down, so does your anxiety, your muscle tension, and even your seizure activity. This isn't magic. It's pharmacology. And it's fast. Unlike antidepressants, which can take weeks to show results, benzodiazepines kick in within an hour. That speed is why they're still used in emergency rooms for status epilepticus and in hospitals to sedate patients before surgery.
Not all benzodiazepines are the same. They come in three flavors based on how long they last in your body. Short-acting ones like triazolam and alprazolam are great for panic attacks or insomnia because they leave your system quickly. Longer-acting ones like diazepam and flurazepam stick around for days, making them better for managing ongoing anxiety or alcohol withdrawal. The choice isn't just about symptoms-it's about matching the drug's half-life to your condition.
The Real Benefits
For many people, benzodiazepines are the only thing that gives them back control. A 2023 survey from the Centre for Addiction and Mental Health (CAMH) found that 60-80% of patients with severe panic disorder saw dramatic improvement within days of starting treatment. For someone terrified of flying, driving, or leaving their house, that kind of relief isn't optional-it's life-saving. Emergency doctors rely on midazolam to stop prolonged seizures. In intensive care units, it's used to keep ventilated patients calm. These aren't fringe uses-they're standard, life-saving practices.
Compared to other treatments, benzodiazepines have no real equal when it comes to speed. SSRIs like fluoxetine or sertraline take 4 to 6 weeks to work. If you're in crisis, that's too long. That's why doctors still prescribe them-for short bursts, for emergencies, for moments when there's no time to wait.
The Hidden Risks
But here's where things get dangerous. The same brain changes that give you relief can also make you dependent. Studies show that after just 4 weeks of daily use, 30-50% of people develop physical dependence. That doesn't mean addiction-it means your body adapts. It starts to need the drug to function normally. When you try to stop, your brain goes into overdrive. Anxiety comes back harder. Insomnia hits like a storm. You might feel your heart racing, your hands shaking, or even have seizures. Withdrawal isn't just uncomfortable-it can be life-threatening.
One of the most overlooked side effects is memory loss. About 23% of people on prescribed doses report gaps in memory during daily activities-forgetting conversations, missing appointments, or not remembering how they got somewhere. This isn't just "getting old." It's a direct effect of the drug on how your brain forms new memories.
And then there's the long-term cost. Benzodiazepines lose their effectiveness after 2-4 weeks of continuous use. Your body builds tolerance. You need more to get the same effect. That's when people start taking extra pills, mixing them with alcohol, or buying them illegally. The Drug Enforcement Administration (DEA) classifies most benzodiazepines as Schedule IV controlled substances for a reason. They're not illegal, but they're tightly watched.
Who’s Most at Risk?
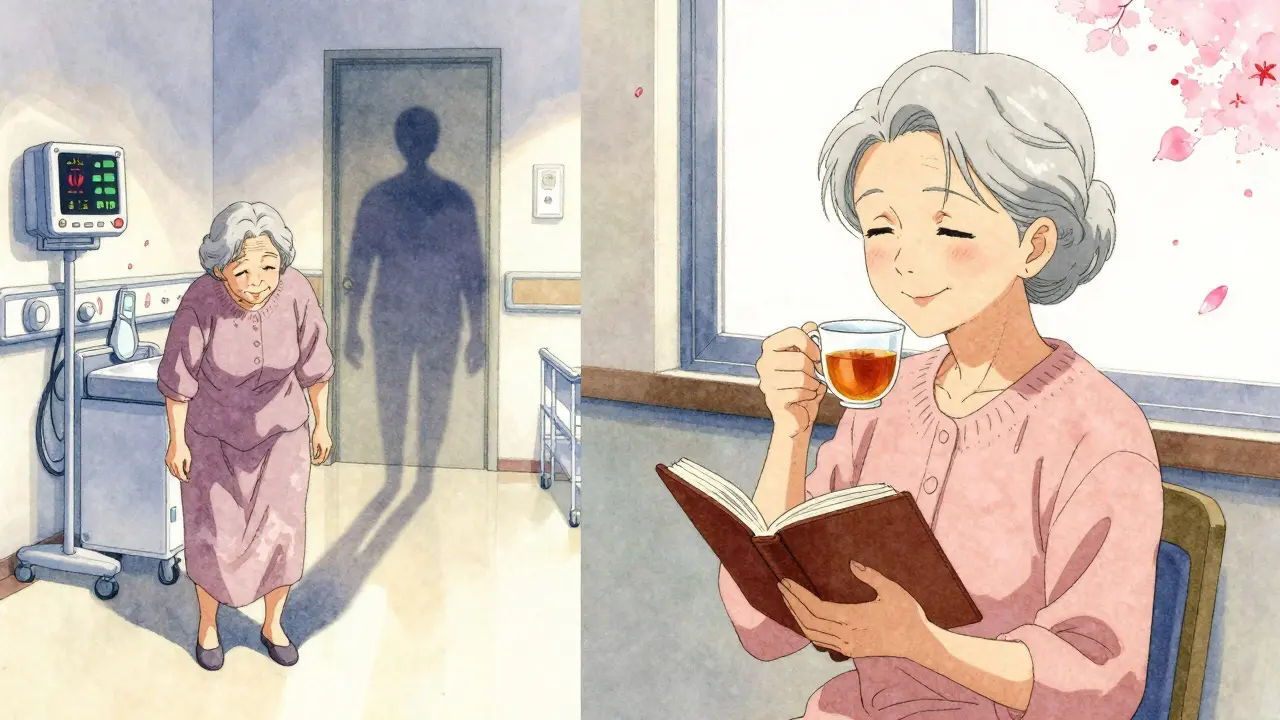
It's not just about how long you take them-it's who you are. Women are prescribed benzodiazepines nearly twice as often as men. Older adults are especially vulnerable. The American Geriatrics Society says people over 65 should avoid them entirely. Why? Because they double the risk of falls and increase the chance of dementia by 32%. Even a single dose can leave an elderly person wobbly, confused, and at risk of breaking a hip.
People with a history of substance use are also at higher risk. If you've struggled with alcohol or opioids before, benzodiazepines can become another way to self-medicate. And because they're so commonly prescribed, many people don't realize they're on them long-term. A 2021 study found that 61% of problematic cases involved patients who took their prescriptions longer than recommended-sometimes for years.
What Should You Do Instead?
The good news? You don't need to live with anxiety forever. Cognitive behavioral therapy for insomnia (CBT-I) works better than sleeping pills in the long run. For anxiety, therapy that helps you reframe thoughts and manage physical symptoms has been shown to be as effective as medication-with no risk of dependence. A 2023 study in JAMA Internal Medicine found that combining low-dose benzodiazepines with CBT reduced long-term dependence by 58% compared to using the drug alone.
Non-benzodiazepine sleep aids like zolpidem are often used for insomnia, but they carry similar risks. Antidepressants like SSRIs are now the gold standard for long-term anxiety treatment. They don't work fast, but they work safely. And unlike benzodiazepines, they don't make you drowsy, foggy, or dependent.

How to Stop Safely
If you've been on benzodiazepines for more than a few weeks, don't just quit. Stopping cold turkey can trigger seizures, hallucinations, or extreme anxiety. The Ashton Manual-the gold standard for tapering-recommends reducing your dose by 5-10% every 1-2 weeks. For someone on a long-term prescription, that process can take 3 to 6 months. It's slow. It's frustrating. But it's the only way to avoid serious withdrawal.
Doctors who prescribe these drugs are now required to complete 40 hours of training every two years on controlled substances. That's because prescribing them isn't just about writing a script-it's about understanding the full cycle: when to start, how long to continue, and how to get off safely. Many clinics now use electronic alerts to flag prescriptions that go beyond 90 days. Kaiser Permanente cut long-term use by 37% just by adding those alerts.
The Future of Benzodiazepines
Global use is still rising. In 2022, the market was worth $1.78 billion. France prescribes them at more than six times the rate of the U.S. But the tide is turning. The FDA added a boxed warning in 2020 about abuse and dependence. The UK's NICE guidelines now say benzodiazepines shouldn't be started for anxiety disorders at all. The trend is clear: these drugs aren't going away, but their role is shrinking.
They'll still be used in emergencies-seizures, surgery, alcohol withdrawal. But chronic anxiety? That's moving to therapy, SSRIs, and lifestyle changes. The future isn't about more pills. It's about smarter, safer ways to heal.
Can you become addicted to benzodiazepines even if you take them as prescribed?
Yes. Addiction means using a drug compulsively despite harm. Physical dependence is different-it means your body adapts to the drug and goes into withdrawal when you stop. You can become physically dependent even if you follow your doctor's instructions exactly. Studies show 30-50% of people taking therapeutic doses for more than 4 weeks develop dependence. That doesn't mean you're an addict, but it does mean stopping suddenly can be dangerous.
How long is it safe to take benzodiazepines?
Most guidelines recommend no more than 2 to 4 weeks for anxiety or insomnia. After that, the benefits decline and the risks rise. Tolerance develops quickly, meaning you need higher doses for the same effect. Long-term use increases the chance of memory problems, falls (especially in older adults), and severe withdrawal. If you need ongoing help, therapy or non-addictive medications like SSRIs are safer choices.
What are the signs of benzodiazepine withdrawal?
Withdrawal symptoms can start within hours or days after stopping and may include intense anxiety, panic attacks, insomnia, tremors, sweating, nausea, muscle pain, dizziness, and heightened sensitivity to light or sound. More severe cases can involve seizures, hallucinations, or delirium. Symptoms can last for weeks or months, especially after long-term use. That's why tapering slowly under medical supervision is critical.
Are there safer alternatives to benzodiazepines for anxiety?
Yes. SSRIs and SNRIs are the first-line treatments for chronic anxiety because they don't cause dependence and have fewer side effects than benzodiazepines. Cognitive behavioral therapy (CBT) is just as effective long-term and has no risk of physical dependence. For sleep problems, CBT-I is more effective than sleeping pills. While benzodiazepines are fast, alternatives are safer and more sustainable.
Why are benzodiazepines still prescribed if they're so risky?
Because they work-fast. For acute panic attacks, severe insomnia, seizures, or alcohol withdrawal, no other drug acts as quickly or reliably. They're essential in emergency medicine and short-term crisis management. The problem isn't their use-it's their overuse and long-term use. When used correctly and sparingly, they save lives. When used as a long-term solution for chronic anxiety, they create new problems.

